they’ll Getcha…getcha, getcha, getcha, getcha… One way or another they’re gonna KILL YA.
So ask yourself, what is in the tube? on the swab? in the needle?

For sometime now, it has been clear that the Elite have an agenda to bring down all the nations by the use of three issues:
- Climate Change/Global Warming
- HEALTHCARE/PLANDEMICS
- ONE WORLD RELGION.
Now, I have posted many articles on the lie that is Climate Change, as well as the lie that is UNITY/One Religion for all. This post is dedicated to the issue in the middle. HEALTHCARE/MEDICAL TYRANNY and PLANDEMICS.
It is true I have several articles about the vaccines, the plan to use pandemics and endemics to control us, about how they used COVID to destroy economies worldwide and how their HEALTHCARE has nothing to do with HEALTH or CARE.
In this Post, we are going to take a look at the diseases themselves and what is going on with them. I have been hearing and reading some very concerning news that they are all ready beginning to lock down cities across our country. I want to know why.
So, I begin with reviewing the different diseases and the numbers of cases. But, don’t get weary before you reach the end. This was an adventure that lead me to things I did not know. Clarification of a lot and verification of a lot. Of course, that often happens when the Holy Spirit leads you.
So stay with me. This post is full of information you should know.
Illegal Immigration Bringing Tuberculosis and Polio to New York
spacer
spacer
spacer
spacer

CDC estimates that each year 48 million people get sick from a foodborne illness, 128,000 are hospitalized, and 3,000 die.
Causes of Food Poisoning
Top 5 Germs Causing Illness, Hospitalizations, and Deaths From Food Eaten in the United States
- Norovirus.
- Salmonella (non-typhoidal)
- Clostridium perfringens.
- Campylobacter.
- Staphylococcus aureus.
- Salmonella can cause salmonellosis and typhoid fever and paratyphoid fever.
- Botulism is most often caused by Clostridium botulinum.
- Some other germs that cause foodborne illness include Cryptosporidium, Cyclospora, hepatitis A virus, Shigella, and Yersinia.
- See a complete A-Z index of foodborne illnesses.
Some foodborne germs can be antimicrobial resistant.
- Antimicrobial resistance happens when germs like bacteria and fungi develop the ability to defeat the drugs designed to kill them. That means the germs are not killed and continue to grow.
- People infected with antimicrobial-resistant germs might have more severe illness and fewer treatment options.
- Although people with a severe infection may need to see a doctor, be prescribed antibiotics, or be hospitalized, people with mild symptoms of food poisoning usually do not need antibiotics to get better.
Bacterial Infections
spacer
The US Centers for Disease Control and Prevention is investigating a salmonella outbreak that has been linked to flour, and it’s urging people not to eat or play with uncooked dough or batter.
A dozen illnesses – including three hospitalizations – have been reported in connection with the outbreak, spanning 11 states. However, the CDC says that the scale of the outbreak is probably much larger than the number of reported cases suggests.
The agency has not identified specific brands of flour involved in the outbreak.
(why not? Now we know that every single item sold today is marked with a barcode that identifies where it originated. how can it be that hard to locate the source of a contaminant? I think it is very likely that they are protecting the corporate owners.)
Most of the patients whom the CDC has interviewed said they had eaten raw dough or batter in the week before falling ill, the timing of which spanned from December to mid-February. Flour was the only common ingredient in the raw dough or batter that was eaten.
Most flour is raw and hasn’t been treated to kill germs that cause food poisoning, according to the CDC. Salmonella bacteria dies when it is cooked or baked, but people can get sick when eating or tasting foods that include raw flour. Raw dough used for crafts and play clay also pose a risk.
To stay safe, the CDC recommends following recipe or package instructions to fully cook cookies, cakes and other foods made with raw flour, and using warm water and soap to wash hands, utensils, countertops and anything else that comes into contact with raw four. People should also use heat-treated flour for homemade playdough.
Symptoms of a salmonella infection include diarrhea, fever and stomach cramps that can start within hours or days of consuming the bacteria. Most people will recover with treatment but should seek immediate attention from a health care provider if they have severe symptoms, symptoms that don’t improve after a few days or signs of dehydration.
spacer
Posted June 13, 2023
CDC, public health and regulatory officials in several states, and the U.S. Food and Drug Administration (FDA) investigated a multistate outbreak of Listeria monocytogenes infections.
Epidemiologic data showed that leafy greens were a likely source of the outbreak. However, there was not enough other data to identify a specific type or producer of leafy greens. (Again, I call BS.)
As of June 13, 2023, this outbreak is over.
Epidemiologic Data
As of June 13, 2023, a total of 19 people infected with the outbreak strain of Listeria were reported from 16 states (see map). Sick people’s samples were collected from July 3, 2018, to March 31, 2023 (see timeline). Seriously?? That is an outbreak? 19 people in 16 states over 5 years?
The true number of sick people in this outbreak is likely higher than the number reported, and the outbreak may not be limited to the states with known illnesses. This is because some people recover without medical care and are not tested for Listeria.
Public health officials collected many different types of information from sick people, including their age, race, ethnicity, other demographics, and the foods they ate in the month before they got sick. This information provided clues to help investigators identify the source of the outbreak.
Sick people ranged in age from less than 1 to 96 years, with a median age of 72, and 63% were female. Among 19 people with race information available, 17 people were White, 1 was African American/Black, and 1 reported “Other” race. Among 19 people with ethnicity information available, two people were Hispanic. Eighteen people were hospitalized, and no deaths were reported.
State and local public health officials interviewed people about the foods they ate in the month before they got sick. Of 14 people who answered questions about leafy greens, 13 (93%) people ate leafy greens, 13 (93%) ate iceberg lettuce, and 10 (71%) ate romaine lettuce. Twelve (86%) people ate packaged salads.
CDC conducted a case-case analysis, comparing foods that sick people in this outbreak reported eating to foods that people sick with Listeria reported eating who were not part of an outbreak. The analysis showed that people in this outbreak were 8 times more likely to eat iceberg lettuce (p=0.035), 5 times more likely to eat romaine lettuce (p=0.038), and 4 times more likely to eat packaged salads (p=0.049) than sick people not in this outbreak. This suggests that leafy greens were a likely source of this outbreak.
Three people ate leafy greens at the long-term care facilities they lived in, and one person ate leafy greens at a hospital they worked in. People bought leafy greens and different brands of packaged salads from several stores.
Laboratory Data
Public health investigators used the PulseNet system to identify illnesses that were part of this outbreak. CDC PulseNet manages a national database of DNA fingerprints of bacteria that cause foodborne illnesses. DNA fingerprinting is performed on bacteria using a method called whole genome sequencing (WGS).
WGS showed that bacteria from sick people’s samples were closely related genetically. This suggests that people in this outbreak got sick from the same food.
Where Sick People Lived
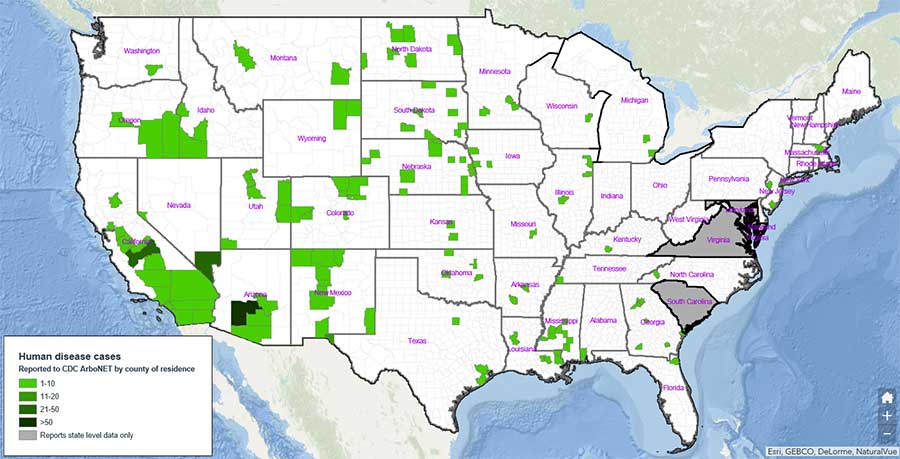
This map shows where the 19 people in this Listeria outbreak lived.
This outbreak may not have been limited to the states with known illnesses, and the true number of sick people is likely higher than the number reported. This is because some people recover without medical care and are not tested for Listeria.
spacer
By Amy Norton HealthDay Reporter

(HEALTHDAY)
FRIDAY, March 24, 2023 (HealthDay News) — E. coli bacteria are an infamous cause of food poisoning, but a new study suggests those same microbes lurking in meat may be behind nearly half a million cases of urinary tract infections (UTIs).
Although E. coli may be best known for spurring outbreaks of food poisoning, most strains of the bacteria are actually harmless. In fact, E. coli lives happily in the human gut, as part of the vast array of beneficial bacteria that make up the body’s “microbiome.”
America’s 25 Healthiest Communities
That, at least, is the source of most UTIs, said study author Lance Price, a microbiologist and professor at George Washington University, in Washington, D.C.
Price’s team found genetic evidence that some UTIs are caused by E. coli in the chicken, turkey and pork that people buy at the grocery store. The bacteria find their way to the urinary tract the same way as other UTI-causing E. coli do — but the source is different.
The researchers estimated that around 8% of UTIs caused by E. coli can be traced to a food source. That would translate to about a half-million such infections among Americans each year, Price noted.
UTIs are especially prevalent among women, who get them up to 30 times more often than men, according to the U.S. Office on Women’s Health. Women are vulnerable largely due to anatomy: The opening to the urethra (the tube through which urine flows) is situated close to the anus — making it easier for E. coli to find its way to the urinary tract.
For the most part, UTIs occur in the bladder and cause symptoms like a frequent urge to urinate, burning during urination and lower belly pain. In a small number of cases, UTIs lead to more serious, even life-threatening, infections if they spread to the kidneys or blood.
So, preventing even a small portion of the infections could have a big payoff, Price said.
The study, published online recently in the journal One Health, is not the first to suggest that foodborne E. coli plays a role in UTIs. A 2005 study, for example, concluded that a multistate outbreak of UTIs — which do not normally occur as outbreaks — was likely caused by contaminated food of “animal origin.”
The new research took a broader, and more extensive, approach, Price explained.
Over the course of a year, the investigators went out every two weeks to buy samples of all available brands of raw chicken, turkey and pork at the nine major grocery chains in Flagstaff, Ariz. They also collected all E. coli samples isolated from patients at the city’s major medical center during the same period.
By analyzing the genomes of E. coli from meat and from patients, the researchers zeroed in on segments of bacterial DNA that are unique to strains that colonize animals that people eat — not people. From there, they developed a mathematical model that predicted the likelihood that E. coli came from a person or from food.
In the end, the model identified 8% of patients as having E. coli infection from meat.
Scaling that to the national level, the researchers estimated that foodborne E. coli could account for around half a million UTIs each year.
A urologist not involved in the study cautioned that the findings do not definitively prove that people in the study contracted UTIs due to undercooked chicken. So, more research is warranted, said Dr. Johanna Figueroa, a urologist at Northwell Health, in New Hyde Park, N.Y.
At the same time, she said, no one would argue against safe cooking and good bathroom hygiene to protect yourself against foodborne E. coli.
Price agreed. That means not only adequately cooking meat, but being vigilant about cross-contamination: Wash your hands after handling raw meat or its packaging, Price said, and keep food preparation surfaces clean.
“I tell people to make the salad, or anything you’re going to eat raw, first — before you even take the meat out of the refrigerator,” Price added.
As for reducing the risk of recurrent UTIs, the standard advice to women is good bathroom hygiene: Wipe “front to back” to help keep E. coli away from the urinary tract. Drinking enough water is also important, Figueroa said, since that dilutes the urine and lowers the concentration of bacteria.
Neither expert advised people with repeat UTIs to go vegetarian. But Figueroa noted that a nutritious diet (including plenty of fruits and vegetables), adequate sleep, exercise and other healthy habits can help support stronger immune function.
On a larger scale, Price said he hopes the findings can ultimately be used by industry. The research points the finger at specific E. coli strains that may be contributing to UTIs, so it may be possible to limit their presence in the food supply, he noted.
spacer
CDC warns of tick-borne illness which may be undiagnosed in nearly half-a-million Americans
spacer
The next pandemic could spring from the US meat supply, new report finds
The next global pandemic could come from the United States.
That’s the sobering message of a report from Harvard Law School and New York University, examining how humans, livestock and wild animals interact here.
Many familiar ‒ and terrifying diseases ‒ originated in animals, including HIV/AIDS, Ebola, Zika, pandemic flu and COVID-19. Some started in other countries, typically on the African or Asian continents. These so-called zoonotic diseases are often blamed on poor hygiene, lack of government oversight, or unsafe practices in those places.
While Americans often think “it couldn’t happen here,” regulations are so loose and interactions so frequent, researchers found, that a virus or another contagious bug could easily jump from animals to people in the U.S., sparking a deadly outbreak. (Scientists have been feverishly working in the Labs to try to create diseases that could spread from animals to humans. GOD had a barrier established to prevent it.)
spacer
 |
 |
spacer
The report, also led by NYU’s Center for Environmental and Animal Protection, highlights several areas of vulnerability, including commercial farms where millions of livestock come into close contact with each other and their handlers; the wild animal trade in which animals are imported with few or no health checks; and the fur trade in which minks and other animals are bred for their coats, with little safety oversight.
All developments of the Industrial Revolution, totally contrary to nature. Greed is an ugly thing and what goes on in the corporate world would horrify the public if they were able to see their disgusting practices.
“Through globalization, we’ve erased seas and mountains and other natural boundaries of disease,” said Linder, an expert in law and animal policy. “We’re mixing animals and pathogens across different continents and circulating at a dizzying and ever-increasing pace.” I am convinced that this is being done deliberately, in order to bring about their global government.
About 10 billion land animals are raised in the U.S., a number which is increasing by about 200 million a year, according to the report. Pigs and poultry, for instance, are raised in higher numbers in the United States than almost anywhere else in the world, the report found, and are the most likely vectors for a particularly lethal outbreak of the flu.
With the help of lab created diseases.
Industry representatives were quick to defend the safety of their practices. Of course, deny, deny, deny that is what abusers always do.
“According to the CDC, the likelihood of spreading an avian disease to a human in the United States is extremely rare,” Ashley Peterson, National Chicken Council senior vice president of scientific and regulatory affairs, said in an emailed statement.
A pork industry group did not immediately return a request for comment.
Workers on pig and poultry farms are particularly vulnerable because of a lack of regulations protecting them, said Delcianna Winders, an associate professor of law and director of the Animal Law and Policy Institute at Vermont Law and Graduate School in Royalton.
“There is virtually no regulation of on-farm raising of animals. There’s limited regulation of the slaughterhouse but it is extremely inadequate and it’s getting worse,” said Winders, who was not involved in the report, but researches a similar area. “Right now, the federal government is deregulating slaughter, rather than increasing oversight.“
Because the mink and larger fur industry does not produce food, it is even less regulated, Linder said.
A different study publishedlast week in “Proceedings of the National Academy of Sciences,” found “that mink, more so than any other farmed species, pose a risk for the emergence of future disease outbreaks and the evolution of future pandemics.” Other studies have shown that mink are susceptible to SARS-CoV-2, the virus that causes COVID-19, and outbreaks were detected on 18 American mink farms during the pandemic’s first two years. At least four Americans, two of whom worked on mink farms, were believed to have been infected by the animals.
Challis Hobbs, Executive Director of the Fur Commission USA, a trade group, said “we unequivocally assert our commitment to the health and safety of our animals, our workforce, and the communities in which we operate.”
The industry, working with the federal government and state agencies, vaccinated 95% of the U.S. mink population beginning summer 2021, he said. The cost was entirely covered by the mink farmers, who also are helping to fund a SARS-CoV-2 surveillance project on mink farms.
“Despite claims from animal rights advocates,” he said, “there is no significant threat to the general public from U.S. farmed mink.
About 220 million live wild animals are imported into the United States every year for pets and other purposes, many without health or safety checks, Linder said.
If someone wants to bring a dog or cat into this country, there’s a process, Linder said. “But if I’m a wildlife importer and I want to bring in 100 wild mammals from South America, I can do that with very little regulation of any kind.” Why is that??
Perhaps the earliest Ebola case, which sparked the outbreak in West Africa from 2013 to 2016, was blamed on bush meat. It’s illegal to import bush meat to the United States, but it’s not illegal to import the same live animals that bush meat comes from, she said. “There are wide gaps.”
Both Linder and Winders also highlighted the lack of industry transparency.
“So much of this is hidden from public view,” Winders said. “There’s so much we don’t know because we’re not monitoring.“
Winders said she’s concerned about how much money the government spends subsidizing and protecting industries she believes put the American public at risk. She hopes Congress will take advantage of this year’s reenactment of the Farm Bill to limit subsidies and impose new safety regulations on animal industries.
“Don’t we see the writing on the wall?” Winders asked. “Scientists are telling us there’s a looming threat of a zoonotic outbreak that could make COVID look like a cakewalk, and we’re still just ignoring it, even after what we’ve gone through over the last couple of years.“
Contact Karen Weintraub at kweintraub@usatoday.com and Adrianna Rodriguez at arodriguez@usatoday.com.
spacer
Flea-borne typhus led to reported deaths in L.A. County ...
Los Angeles Times
spacer
Polio Detected in NY County’s Wastewater Again, 1st Time ...
NBC New York
By Tom Shea
Scientists are finding ways to curb the future community spread of infectious diseases like coronavirus, monkeypox and polio by investigating the wastewater found underground. NBC New York’s Linda Gaudino brings you to the sewers to uncover the process.
For the first time since Oct. 2022, the New York State Department of Health confirmed that polio had been detected in local wastewater from Rockland County.
In a Thursday release, the county said that there was a single positive result that had been collected in February, and that so far, no other samples have had any detection of the virus. County officials said that any residents who are unvaccinated should act quickly to best protect themselves.
spacer
Polio in the United States
Centers for Disease Control and Prevention (.gov)
August 3, 2022 Polio was once one of the most feared diseases in the United States. Thanks to vaccination, wild poliovirus has been eliminated in this country.
The best way to keep people safe from polio is to maintain high immunity (protection) against polio in the population through vaccination.
Poliovirus detections in wastewater should be a rare event; work with your state and/or local health department to consider whether to initiate this type of testing.
CDC Wastewater Investigation, 2023
CDC is working with select jurisdictions to strategically expand wastewater testing for poliovirus in counties with potentially low polio vaccination coverage.
A polio case identified in New York last month is “just the very, very tip of the iceberg” and an indication there “must be several hundred cases in the community circulating,” a senior official with the US Centers for Disease Control and Prevention told CNN on Wednesday.
The case was found In Rockland County, which has a stunningly low polio vaccination rate. Dr. José Romero, director of the CDC’s National Center for Immunization and Respiratory Diseases, noted that the majority of people with polio don’t have symptoms and so can spread the virus without knowing it.
“There are a number of individuals in the community that have been infected with poliovirus. They are shedding the virus,” he said. “The spread is always a possibility because the spread is going to be silent.”
A team of CDC disease detectives traveled last week from agency headquarters in Atlanta to Rockland County, and they are “quite nervous” that polio “could mushroom out of control very quickly and we could have a crisis on our hands,” said a community health leader who has met with the team.
“They are – what is the opposite of cautiously optimistic?” said another community leader, an expert in vaccine education, who has also met with the CDC team in Rockland County. Both leaders requested anonymity because they are not authorized to speak publicly.
Polio can cause incurable paralysis and death, but most people in the US are protected, thanks to vaccination. Others, however, may be vulnerable to the virus for a variety of reasons.
Unvaccinated and undervaccinated people are vulnerable, and polio vaccination rates in Rockland County and neighboring Orange County, just north of New York City, are about 60%, compared with 93% nationwide, by age 2. Immune-compromised people can be vulnerable even if they are fully vaccinated.
Romero said the CDC is considering a variety of options to protect people from polio, including offering children in the area an extra shot of the vaccine, as UK health authorities are doing now in London, or recommending extra doses to certain groups of adults.
spacer
Chicago Department of Public Health Begins Wastewater …
City of Chicago (.gov)
This effort is a collaboration between CDPH (Chicago Department of Public Health) and scientists from the University of Illinois Chicago, the Regional Innovative Public Health Laboratory at Rush University Medical Center, the University of Illinois System’s Discovery Partner Institute, the Illinois Department of Public Health, the Metropolitan Water Reclamation District of Greater Chicago, and the Centers for Disease Control and Prevention. As part of this surveillance, wastewater samples will be routinely collected and processed for laboratory testing for poliovirus to see if poliovirus is present and understand if the type of poliovirus found is of concern.
While no case of paralytic polio has been identified in Chicago or Illinois at this time, CDPH is proactively building its local capacity to detect and respond to any potential case of polio. The best way to protect everyone from polio is to maintain high immunity against poliovirus in the population through vaccination.
Finding poliovirus in wastewater indicates that someone in the community is shedding poliovirus. Wastewater data cannot be used to determine or identify who is infected or how many people or households are affected, but it can enhance other data and surveillance methods used to prevent polio. Not all potential detections will be cause for concern. However, if specific strains of poliovirus are found in communities that have low vaccination rates, it can spread among unvaccinated individuals, putting them at risk for becoming infected and developing polio. Anyone who is unvaccinated or incompletely vaccinated is at risk for developing paralysis if infected with poliovirus.
“Polio has been eradicated in the US since 1979; however, a recent case in 2022 in New York State highlights the importance of rapid detection to interrupt any new outbreaks and strengthen routine immunization, which is the best national defense against polio,” said CDPH Deputy Commissioner Massimo Pacilli.
Polio can lead to permanent paralysis of the arms and legs and can be fatal due to paralysis in the muscles used to breathe or swallow. Most people infected with the virus do not have any symptoms, though some will have flu-like symptoms, like sore throat, fever, tiredness, nausea, and stomach pain. One in 25 people with poliovirus infection will get meningitis and about one in 200 will become paralyzed. While there is no cure for polio, it is preventable through safe and effective immunization. In the United States, the risk of getting polio is extremely low. Most people are vaccinated against polio during childhood, and this provides protection against serious illness, including paralytic polio. Studies suggest people who completed their polio vaccination during childhood are likely protected throughout adulthood.
Improving vaccination coverage, rapid reporting, and national case surveillance are the keys to preventing cases of paralytic polio. The complete recommended polio vaccination series is extremely effective in preventing paralytic polio, and the vaccine protects against severe disease in almost everyone who has received the recommended doses. Illinois’ Vaccines for Children (VFC) program offers vaccines at no cost to eligible children through health care providers enrolled in the program, including uninsured, underinsured and Medicaid eligible children. You can find a vaccine provider by visiting http://vfc.illinois.gov/search/. Additionally, CDPH operates two immunization clinics where children and young adults 18 years of age and under can get required and recommended vaccinations at no cost. Get more information online from CDPH about the clinics, including locations and hours: https://www.chicago.gov/city/en/depts/cdph/supp_info/health-protection/immunizations_walk-inclinics.html
Additionally, adults and children traveling to countries where poliovirus is circulating, should get updated polio vaccinations before travel. Primary care providers, travel clinics as well as pharmacies can provide pre-travel vaccinations to adults.
CDPH’s current program routinely tests wastewater samples across the city of Chicago to monitor SARS-CoV-2 and influenza and provides monthly updates for the public on its website: https://www.chicago.gov/city/en/sites/covid-19/home/covid-19-wastewater-surveillance.html Additional SARS-CoV-2 wastewater data for the greater Chicago area is available at https://iwss.uillinois.edu/.
spacer
Half of migrants piling into NYC not vaxxed for polio, top doc warns
New York Post
Apr 16, 2023 —
A startling 50% of migrants streaming into the Big Apple are not vaccinated against the contagious and potentially deadly poliovirus, city Health Commissioner Ashwin Vasan recently revealed — as he urged doctors to help prevent a public health emergency, The Post has learned.
Vasan also said the new migrants come from, or pass through, countries with high rates of infectious tuberculosis — and noted there’ve been outbreaks of chickenpox in shelters housing the newcomers.
“More than 50,000 people have come to New York City (NYC) in the past year shortly after crossing the U.S.-Mexico border. As more people arrive and many make NYC their home, the scale and scope of need continues to grow,” Vasan said in an eight-page letter, dated April 11, sent to physicians and other health care providers. A copy was obtained by The Post.
“There is always a risk to public health when people are not vaccinated against important infectious diseases, such as measles and polio,” Varma said told The Post on Sunday.
“That said, the risk is not immediate, since there are high levels of vaccination among children and adults among current New Yorkers. As the Commissioner says, it is critical that the City work to provide newly arrived persons with medical care, and ensure that healthcare providers catch up newly arrived persons on their vaccinations, just as happens routinely for anyone accepted into the US through the regular immigrant or refugee resettlement programs.”
“Children should be screened and vaccinated urgently with all needed recommended immunizations, including those required for school attendance. Both influenza and COVID-19 vaccination should be offered to everyone age 6 months and older,” Vasan wrote.
He also said it was important to test for tuberculosis, an infectious bacterial disease characterized by the growth of nodules in the tissues, especially the lungs.
“Many people who recently arrived in NYC have lived in or traveled through countries with high rates of TB,” Vasan said.
He said people with symptoms of active TB should be promptly evaluated and tested, including chest X-rays.
The letter said migrants have been infected with chicken pox.
“An outbreak of varicella is occurring among families who recently arrived and are residing in shelters and other facilities in NYC. Most cases have been among unvaccinated children, but cases have also occurred among young adults,” the letter said.
Varicella-Zoster Virus (Chickenpox and Shingles)Varicella-zoster is a herpes virus that causes chickenpox, a common childhood illness. It is highly contagious. If an adult develops chickenpox, the illness may be more severe. After a person has had chickenpox, the varicella-zoster virus can remain inactive in the body for many years. |
Chickenpox is a highly contagious and causes an itchy, blister-like rash on the skin; it is not considered life-threatening.
“Vaccinate children and adults with no or an unknown history of varicella or vaccination urgently,” Vasan said.
Typically, individual cases of varicella don’t need to be reported to the Health Department.
But the commissioner said because of the recent outbreak with migrants, chickenpox cases in shelters need to be reported to the Health Department Provider Access Line.
FOR IMMEDIATE RELEASE
Date: May 15 2023
Contact: Jon Ebelt, Communications Director, DPHHS, (406) 444-0936, (406) 461-3757
jebelt@mt.gov
Chickenpox Cases on the Rise in Youth
Most cases related to shingles exposure, health officials encourage chickenpox vaccination
Department of Public Health and Human Services (DPHHS) officials are reporting a recent increase in the number of cases of chickenpox reported in school-aged children.
And, at least half of these infections were acquired from an adult family member with shingles. Chickenpox, or varicella, can be a serious illness and is easily preventable with vaccination.
“The best way to protect yourself and your child from chickenpox is vaccination,” says Jessica Lopeman, a registered nurse and epidemiologist with DPHHS.
In 2022, there were 23 reported cases of chickenpox in Montana. Cases ranged in individuals from age 1 to over 65. One infant and one young adult required hospitalization.
Early numbers from 2023 show 18 reported cases of chickenpox with no known hospitalizations. Only six cases were reported during the same period last year, which is a 200% increase in cases year-to-date. Shingles is not a reportable condition; therefore, there is no data on the number of cases last year in Montana.
Shingles is a reactivation of the varicella virus, the virus that causes chickenpox. It occurs in 1 of 3 persons who have had chickenpox in their lifetime. Shingles has a rash that presents as red bumps and blisters, usually in a narrow area on one side of the body. This rash may be itchy or painful and is contagious until it has scabbed over completely and can be transmitted by direct contact.
However, the virus is almost exclusively transmitted to people who are not vaccinated for chickenpox or have never had it in the past.
Transmission of the virus may be prevented by covering the shingles rash to prevent contact. The incidence of shingles increases with age, and vaccination against shingles is recommended for persons 50 years and older.
Chickenpox is an illness with a rash and a fever. Like shingles, chicken pox is also caused by the varicella virus. The rash usually appears 14 to 16 days following exposure to the varicella virus, but can be as early as 10 days or as long as 21 days.
It is highly contagious to those who are not immune, especially those who have not been vaccinated with two doses of chickenpox vaccine. Chickenpox can also be serious, even life-threatening, especially in babies, adolescents, adults, pregnant women and people with weakened immune systems. The vaccine is excellent at preventing chickenpox by providing 98.3% effectiveness.
“With the recent rise in cases related to shingles exposures, DPHHS is reminding parents and grandparents that shingles can cause chickenpox in unvaccinated persons who have not previously had the virus,” Lopeman said. “It’s important that children are up-to-date on vaccines, including the chickenpox vaccine, and if someone does develop shingles, keep the shingles rash covered to prevent exposure and transmission of the varicella virus.”
spacer
Measles (Rubeola)
Measles Cases and Outbreaks USA
CDC updates this page monthly.
Measles cases in 2023
As of August 3, 2023, a total of 19 measles cases were reported by 13 jurisdictions. *
Measles cases in 2022
From January 1 to December 31, 2022, a total of 121 measles cases were reported by 6 jurisdictions. *
Measles cases in 2021
From January 1 to December 31, 2021, a total of 49 measles cases were reported by 5 jurisdictions. *
Measles cases in 2020
From January 1 to December 31, 2020, 13 individual cases of measles were confirmed in 8 jurisdictions.*
*Jurisdictions refer to any of the 50 states, New York City, and the District of Columbia.
Measles cases in 2019
- From January 1 to December 31, 2019, 1,274* individual cases of measles were confirmed in 31 states.
- This is the greatest number of cases reported in the U.S. since 1992. The majority of cases were among people who were not vaccinated against measles. Measles is more likely to spread and cause outbreaks in U.S. communities where groups of people are unvaccinated.
- For more information please see the following reports:
- Increase in Measles Cases – United States, January 1-April 26, 2019 MMWR. May 3, 2019
- National Update on Measles Cases and Outbreaks – United States, January 1-October 1, 2019. MMWR. October 11, 2019

Did you know that measles can be found around the world?
Number of measles cases reported by year
2010-2023* (as of June 8, 2023)
spacer
Malaria cases in Florida and Texas prompt CDC warning

Malaria cases in the US are on the rise: Your visual guide to symptoms and prevention
A public health alert was issued by the Centers for Disease Control and Prevention in June to advise doctors, public health authorities and the public about the risk.
Seven of the cases were identified in Sarasota County, Florida, and one was identified in Cameron County, Texas. None of the patients had traveled outside the state before falling ill.

Can’t see our graphics? Click to reload.
How often is malaria seen in the U.S.?
Malaria was declared eliminated as a major national public health problem in 1951. Now about 2,000 malaria cases are reported in the U.S. each year, typically in returning travelers. Florida and Texas identified 156 cases of malaria total in 2021; all were from returned travelers.

Rhoel Dinglasan, a professor of infectious diseases at the University of Florida’s College of Veterinary Medicine, told the Sarasota Herald-Tribune that cases of locally acquired malaria are not common. The last outbreak of malaria cases in the country was in 2003, when Palm Beach County recorded eight such cases.
Malaria is still a significant global problem even though it has been eradicated in many nations, including in the U.S., and there is no known method of transmission.
The majority of malaria cases and fatalities are found in Africa, where plasmodium faciparum, the most dangerous and widespread malaria parasite, is common. Only a few locations in other regions have transmission.

How is malaria spread?
Malaria is a serious and sometimes life-threatening disease caused by the bite of a female mosquito from the genus Anopheles, the vector that transmits malaria.
Most mosquitoes don’t carry disease. Those that do are called vectors. Among vector-borne diseases: West Nile virus, encephalitis, malaria, dengue fever and chikungunya in humans, or heartworm parasites in dogs.

How it can spread to humans:
When a mosquito bites
A stealth attack: A mosquito releases a substance in its saliva to numb the skin so people don’t feel its bite.
Infection: Diseases such as malaria are found in the mosquito’s saliva.

Feeding: A mosquito uses its proboscis to pierce the skin and locate a blood vessel. The mosquito releases substances that prevent blood from clotting so it can feed longer. Mosquitoes can feed up to 10 minutes.
The itch: The immune system releases histamine to fight the presence of the invading bodies in the skin. The skin swells, making a red itchy bump after a mosquito bite.
What are the signs and symptoms of malaria?
Chills, fever, headache, nausea, body aches and diarrhea are a few of the common malaria symptoms, which are similar to those of the flu, common cold and COVID-19.
The most common symptoms are fever, chills, headaches, muscle aches and fatigue. These symptoms typically occur seven to 30 days after people are infected with the parasite. However, if the infection is untreated, more severe symptoms may appear, including impaired consciousness, difficulty breathing, convulsions, abnormal bleeding and more, which can ultimately lead to death.

How do you protect yourself against malaria?
The CDC recommends using “mosquito avoidance measures” when going outside, including:
- Using EPA-approved mosquito repellent on skin and clothes.
- Wearing long-sleeved shirts and pants, especially at night.
- Staying in well-screened areas.
- Sleeping under an insecticide-treated bed net when camping.
When traveling out of the country, especially to sub-Saharan Africa, the Indian subcontinent, Southeast Asia or tropical South and Central America, consult your doctor about what vaccines and medicines you can take to prevent diseases. Antimalarials help prevent malaria and are available only by prescription.

Contributing: Cheryl McCloud of the Florida Digital Optimization Team and Anne Snabes of the Sarasota Herald-Tribune; The Associated Press
spacer
Meningitis – Meningococcal Disease
Surveillance
Due to recent reports of β-lactamase-producing N. meningitidis serogroup Y in the United States, including 11 cases also resistant to ciprofloxacin:
- Healthcare providers should ascertain susceptibility of meningococcal isolates to penicillin before using penicillin or ampicillin for treatment.
- Clinicians and public health staff should consider antimicrobial susceptibility testing (AST) on meningococcal isolates to inform prophylaxis decisions if their state has reported a case of meningococcal disease caused by ciprofloxacin-resistant strains within the past 2 years.
- Update prophylaxis practices around N. meningitidis cases as needed based on detection of ciprofloxacin-resistance cases.
- View CDC guidance on changing prophylaxis antibiotics in areas with ciprofloxacin resistance.
- State and territorial health departments are asked to
- Continue submitting all meningococcal isolates to CDC for AST and whole genome sequencing
- Report any suspected meningococcal treatment or prophylaxis failures
- Complete a supplemental case report form [2 pages] for cases with isolates determined to be β-lactamase screen-positive or ciprofloxacin-resistant; forms can be submitted to CDC via secure email (meningnet@cdc.gov) or FTP site
Rates of meningococcal disease are at historic lows in the United States. Tracking for meningococcal disease is very good in this country. Health departments respond to every case of meningococcal disease and implement control measures to reduce spread of the disease.
Disease trends
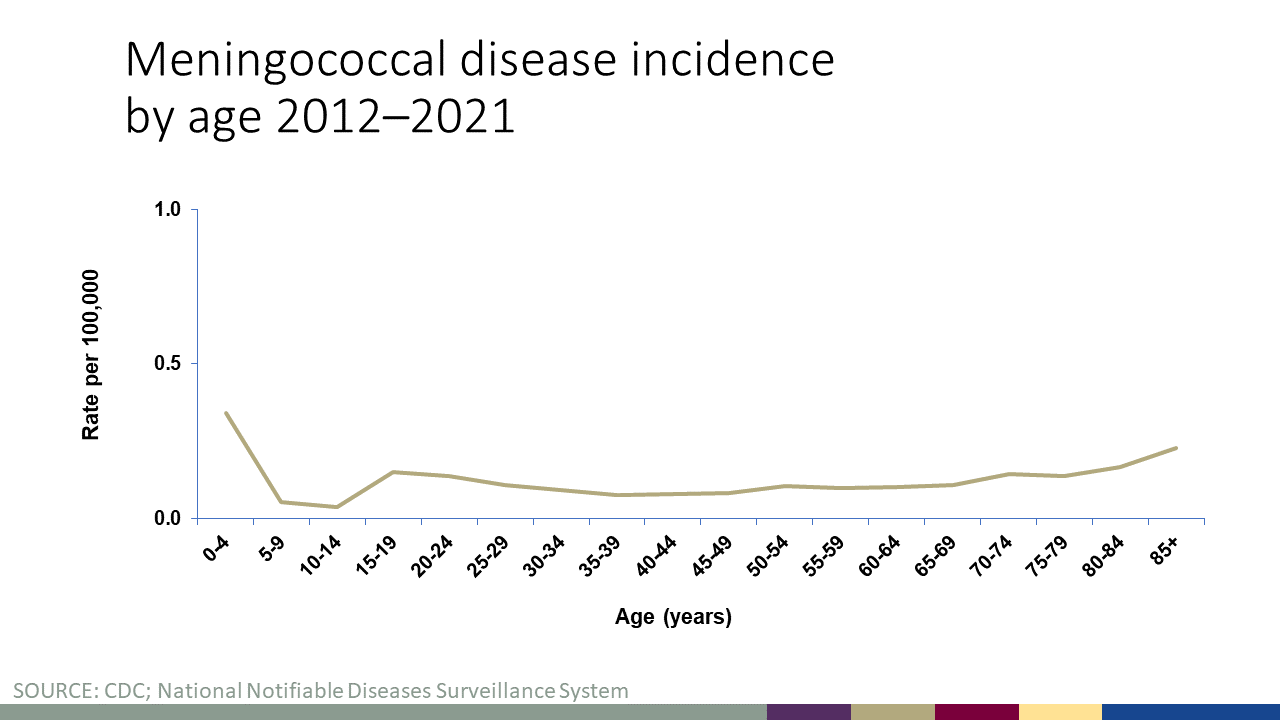
Rates of meningococcal disease have declined in the United States since the 1990s and remain low today. In 2021, there were about 210 total cases of meningococcal disease reported (See Figure 1). Anyone can get meningococcal disease, but rates of disease are highest in children younger than 1 year old, followed by a second peak in adolescence. Among adolescents and young adults, those 16 through 23 years old have the highest rates of meningococcal disease (See Figure 2). The proportion of cases caused by each serogroup varies by age group (See Figure 3).
Meningococcal disease is also seasonal: the number of cases generally peaks each year in January, February, and March.
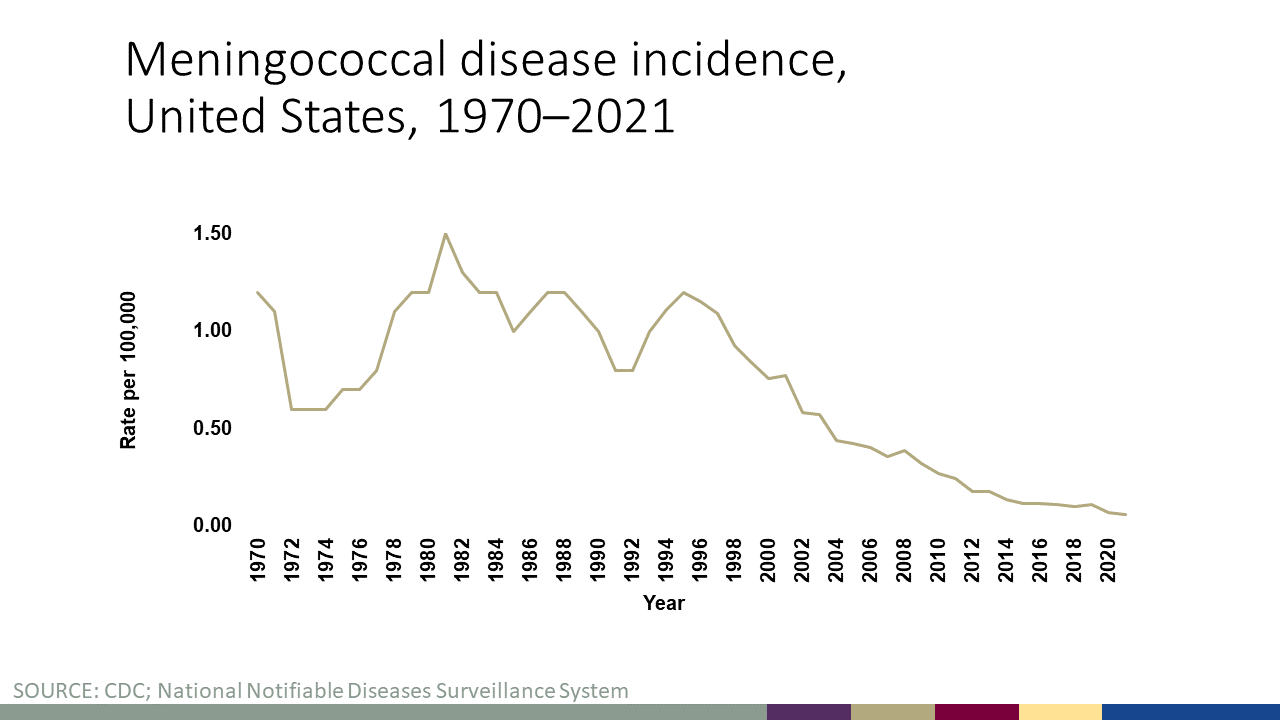
Figure 1 shows incidence rates (per 100,000 persons) of meningococcal disease in the United States by year from 1970 to 2021. The incidence rate began declining in 1995 and has remained low in 2021. View data for this chart.
Figure 2 shows incidence rates (per 100,000 persons) of meningococcal disease by age group from 2011 to 2021. Infants, young adults, and adults >80 years of age have the highest rates of meningococcal disease in the United States. View data for this chart.
DC Health (.gov)
June 15, 2023 – Outbreak of Suspected Fungal Meningitis in U.S. Patients who Underwent Surgical Procedures under Epidural Anesthesia in Matamoros, Mexico
The Centers for Disease Control and Prevention (CDC) issued a Health Advisory on May 17, 2023 and a follow up Health Update on June 1, 2023 about a fungal meningitis outbreak involving patients from the United States and Mexico who underwent cosmetic procedures under epidural anesthesia at two clinics in the city of Matamoros, Tamaulipas state, Mexico.
The first health advisory was released after CDC received multiple reports of U.S patients being hospitalized in Texas following cosmetic procedures. At that time, the causative organism was unknown, however one patient had elevated levels of (1,3)-beta-D-glucan detected in their cerebrospinal fluid (CSF), a marker of fungal infection. By June 1, 2023, three U.S. laboratories in collaboration with the Mexican national laboratory had detected fungal signals consistent with Fusarium solani species complex from the CSF of patients receiving follow-up care in Mexico or United States. More than 200 residents in 25 U.S. states and jurisdictions have been identified at risk for fungal meningitis because they received epidural anesthesia at the affected clinics in 2023. As of June 14, 4 US patients have died. There have been no confirmed cases to-date in the District of Columbia.
This health notice provides information about the ongoing fungal meningitis outbreak and highlights interim recommendations for diagnosis and treatment. All patients who received procedures under epidural anesthesia at River Side Surgical Center or Clinica K-3 since January 1, 2023, regardless of symptoms, should be evaluated for fungal meningitis including a lumbar puncture +/- an MRI of the brain.
The US Centers for Disease Control and Prevention and Florida Department of Health are investigating “one of the worst outbreaks of meningococcal disease among gay and bisexual men in U.S. history,” the CDC said Wednesday.
The CDC said Thursday there have been 26 cases and seven deaths from meningococcal disease in Florida during the investigation period. Among those, 24 cases and six deaths were in men who have sex with men.
The CDC says the outbreak is “primarily among gay, bisexual, and other men who have sex with men, including those living with HIV. Recent data show that about half of the cases associated with this outbreak are among Hispanic men. This outbreak is mostly affecting people who live in Florida but has also affected some people who have traveled to Florida.
Meningococcal disease includes meningitis – infections of the lining of the brain and spinal cord – and bloodstream infections. “Meningococcal disease can affect anyone and can be deadly,” the CDC said in its statement.
The bacteria is spread through sharing respiratory or throat secretions, such as saliva or spit. It normally takes close or lengthy contact, for example kissing or being close to someone who is coughing, to spread the bacteria.
CDC is recommending that gay, bisexual and other men who have sex with men get the meningococcal vaccine if they live in Florida, or talk to their health care provider if they are traveling to the state. For those who live with HIV, health officials are emphasizing the importance of routine vaccination.
“Getting vaccinated against meningococcal disease is the best way to prevent this serious illness, which can quickly become deadly,” said Dr. José R. Romero, director of the National Center for Immunization and Respiratory Diseases, in the CDC news release. “Because of the outbreak in Florida, and the number of Pride events being held across the state in coming weeks, it’s important that gay and bisexual men who live in Florida get vaccinated, and those traveling to Florida talk to their healthcare provider about getting a MenACWY vaccine.”
According to the CDC, the outbreak affecting men who have sex with men is caused by serogroup C. There is also an unrelated serogroup B cluster among college and university students in one county.
The meningococcal disease outbreak update comes as the CDC has been tracking an unusual outbreak of monkeypox in countries where the disease is not endemic, including the United States. The CDC reports has reported 142 orthopoxvirus cases in the United States, including 13 in Florida.
The threat to the general US population is low, the CDC says, but there are notably high numbers of monkeypox cases among gay, bisexual, and other men who have sex with men. “However, anyone who has been in close contact with someone who has monkeypox is at risk,” the CDC notes.
Clarification: On Thursday, the CDC updated and corrected the total number of cases and deaths from meningococcal disease in Florida, including the number among men who have sex with men.
spacer
Viral meningitis
Viral meningitis is more common than bacterial meningitis and, although rarely life-threatening, can make people very unwell. For some, the after-effects can be life-changing
The facts
- Thousands of cases occur every year
- Anyone can get viral meningitis but it is most common in babies and young children
- Viral meningitis symptoms can be similar to those of bacterial meningitis, so it is essential to seek urgent medical help if concerned
- Many different viruses can cause meningitis – enteroviruses are the most common cause
- Is viral meningitis contagious? It is not generally considered to be contagious; contact with someone who has the illness does not usually increase the risk of disease to others. Linked cases of viral meningitis are extremely unusual and almost all cases occur alone
- There is no specific treatment for most cases of viral meningitis. Patients need to be hydrated with fluids, given painkillers and allowed to rest in order to recover. Antibiotics are not effective against viruses. However, in some instances, antibiotics may be started on admission to hospital because the cause of meningitis is not known. Antibiotics are usually discontinued once diagnosed
- Although most people will make a full recovery, the recovery process can be slow. Some can be left with serious and life-changing after-effects
- After-effects can include headaches, exhaustion and memory loss
- Although there aren’t vaccines to prevent most cases, the MMR vaccine, which is given as part of the UK routine immunisation schedule, protects against measles, mumps and rubella viral infections. Prior to the use of this vaccine, mumps was a common cause of viral in children
For the full facts, download our free viral meningitis fact sheet.
The impact
Many people who experience viral meningitis feel that they are dismissed as having the ‘milder’ form of meningitis. Very little is understood about the recovery and after-effects. In response, we carried out a survey, with over 450 sufferers responding. The results (attached to the viral meningitis fact sheet) show the real impact viral meningitis can have.
Been affected by viral meningitis?
Don’t face meningitis alone. Call our Meningitis Helpline on 0808 80 10 388 to speak to our experienced staff. You can access our free support or ask us any questions. Whatever your experience, whenever it was, please get in touch. Our support is for life.
spacer
Hepatitis
2023 Viral Hepatitis National Progress Report Overview
New hepatitis B virus infections declined in 2020 and 2021. Although the two hepatitis B indicators for new infections met the annual target for 2021, it is difficult to determine to what degree the lower rates are attributable to true reductions in disease burden versus impact of the COVID-19 pandemic on access to healthcare, hepatitis testing, and health department capacity to perform viral hepatitis case investigations. The indicators for hepatitis B-related deaths did not meet the annual targets in 2021; however, rates of hepatitis B-related deaths may have been impacted by the increase in overall deaths during the COVID-19 pandemic. Continued efforts are needed to implement CDC’s new, expanded hepatitis B vaccination recommendations and improve appropriate testing and linkage to care.
While the COVID-19 pandemic also likely reduced detection and reporting of new hepatitis C virus (HCV) infections, the impact has been tempered by the introduction of a more sensitive hepatitis C surveillance case definition in 2020, which was designed to classify acute hepatitis C cases more accurately for surveillance. Increases in injection drug use related to the nation’s drug crisis have contributed to annual increases in new HCV infections. To promote health and reduce ongoing transmission, efforts must continue to connect all people experiencing cases of new or chronic hepatitis C to well-tolerated, short-course curative treatment, and connect people who inject drugs to harm reduction services, including syringe services programs and medication for substance use disorder treatment.
Continued efforts are needed to identify new and chronic infections and ensure all people with hepatitis C receive treatment. Death rates among non-Hispanic Black and non-Hispanic American Indian/Alaska Native (AI/AN) populations remain higher than the national rate, with little progress toward the 2025 target for non-Hispanic AI/AN persons since 2017.
spacer
Hepatitis A
Hepatitis is a viral infection of the liver that causes liver inflammation, according to the U.S. Centers for Disease Control and Prevention. A hepatitis A infection is caused by the hepatitis A virus (HAV), which is very contagious, although there is a vaccine available to prevent it.
America’s 25 Healthiest Communities
“Hepatitis A is spread through contaminated food and water, not through blood or sexual intercourse,” explained Dr. Melissa Jenkins, chief of the division of infectious diseases at Cleveland’s MetroHealth Medical Center.
The CDC notes that HAV may also be transmitted through close contact with someone who has been infected with the virus.
Hepatitis A symptoms may last up to two months and include: Fatigue; Nausea; Abdominal pain; Jaundice
“There are no treatments for hepatitis A, except for supportive care [such as] medication for nausea [and] intravenous fluids,” explained Jenkins, who is also an associate professor at Case Western Reserve University School of Medicine, in Cleveland.
She added that “hepatitis A does not cause a chronic infection like hepatitis B and C. Once people recover from hepatitis A, they do not have any long-term liver complications and are immune.”
Hepatitis B
Like hepatitis A, hepatitis B is vaccine preventable. The CDC states that it’s caused by the hepatitis B virus (HBV).
Jenkins explained that HBV “is spread through contact with blood or through sexual intercourse. It can also be spread from mother to child.”
According to the CDC, symptoms of HBV may include:
|
|
|
“Most people who catch it do not have any symptoms at the time of infection, but some will have symptoms like we see with hepatitis C,” Jenkins noted.
- An immunoglobin injection within 24 hours of infection
- Supportive care for acute (short-term) infections, including rest, fluids and monitoring of the infection
Treatments for chronic (long-term) HBV infection may include:
- Antiviral medications
- Interferon injections
- A liver transplant if the virus progresses and causes severe liver damage
“About 5% to 10% of adults do develop a chronic infection with hepatitis B. If people get hepatitis B as a child, it is much more likely that they will develop a chronic infection,” Jenkins said.
“Not all people with chronic infection need treatment right away, but they need to see a doctor regularly to check their status,” she advised.
Hepatitis C
The CDCsays that hepatitis C is unique from hepatitis A and B in that over half the infections are long-term (chronic), and there’s also no vaccine for it. The infection is caused by the hepatitis C virus (HCV).
Having symptoms of acute HCV is not common, but you may experience:
|
|
|
Chronic HCV symptoms are also uncommon but may include: Chronic fatigue; Depression
“Hepatitis C is spread through contact with someone else’s blood,” Jenkins explained. “Current ways people get it are through sharing needles or paraphernalia for injecting or snorting drugs; tattoos, especially ones done in non-professional settings; or occupational exposures, like a health care worker who has a needlestick.”
She added that it may also be transmitted from mother to child during pregnancy, but “is not transmitted very well through sex between a man and woman. Sex between men has a much higher chance of transmitting hepatitis C.”
According to the CDC and Hepatitis C Online, there are a number of antiviral medications available to treat HCV. In more severe cases, it may also be treated with liver transplant surgery.
Hepatitis D
Only people who have had hepatitis B may contract the hepatitis D virus (HDV). For this reason, it’s known as a “satellite virus” according to the CDC. It also has symptoms similar to HBV.
“This is a rapidly progressive disease,” explained Hepatitis B Foundation medical director Dr. Robert Gish, in a Liver Foundation webinar. He advised that this is why all patients with HBV should also be tested for HDV.
The CDC states that the only treatment for HDV is a drug called pegylated interferon alpha.
Hepatitis E
“Hepatitis E is very similar to hepatitis A. It’s spread through contaminated food and water,” said Jenkins.
She noted that the following symptoms may indicate a hepatitis E infection:
|
|
“There are no treatments for hepatitis E other than supportive care,” Jenkins explained, although she also said it’s not a common infection in the United States.
According to the CDC, most people make a full recovery from hepatitis E virus (HEV) infection.
SOURCE: Melissa Jenkins, MD, chief, division of infectious diseases, MetroHealth Medical Center, and associate professor, Case Western Reserve University School of Medicine, Cleveland, Ohio
Copyright © 2023 HealthDay. All rights reserved.
spacer
When hearing about hepatitis A, many people think about contaminated food and water. However, in the United States, hepatitis A is more commonly spread from person to person. Since March 2017, CDC’s Division of Viral Hepatitis (DVH) has been assisting multiple state and local health departments with hepatitis A outbreaks, spread through person-to-person contact.
The hepatitis A vaccine is the best way to prevent hepatitis A virus (HAV) infection
- The following groups are at highest risk for acquiring HAV infection or developing serious complications from HAV infection in these outbreaks and should be offered the hepatitis A vaccine in order to prevent or control an outbreak:
- People who use drugs (injection or non-injection)
- People experiencing unstable housing or homelessness
- Men who have sex with men (MSM)
- People who are currently or were recently incarcerated
- People with chronic liver disease, including cirrhosis, hepatitis B, or hepatitis C
- One dose of single-antigen hepatitis A vaccine has been shown to control outbreaks of hepatitis A.1,2
- Pre-vaccination serologic testing is not required to administer hepatitis A vaccine. Vaccinations should not be postponed if vaccination history cannot be obtained or records are unavailable.
CDC has provided outbreak-specific considerations for hepatitis A vaccine administration and has updated its overall recommendations on the prevention of hepatitis A virus infection in the United States.
Since the outbreaks were first identified in 2016, 37 states have publicly reported the following as of August 4, 2023:
- Cases: 44,903
- Hospitalizations: 27,435 (61%)
- Deaths: 423

spacer

A new recommendation from the US Centers for Disease Control and Prevention says all adults should be screened at least once in their lifetime for hepatitis B, an illness that’s linked to liver disease and cancer.
The agency estimates 580,000 to 2.4 million people live with hepatitis B, known as HBV, and two-thirds might not know about their infection. Many people infected with hepatitis B clear the virus, but acute infection can lead to chronic hepatitis B, which is linked to increased risk of liver cancer and cirrhosis. People with chronic hepatitis B are 70 to 85% more likely to die early.
“Chronic HBV infection can lead to substantial morbidity and mortality but is detectable before the development of severe liver disease using reliable and inexpensive screening tests,” the agency said in a report released Thursday.
Hepatitis B spreads through contact with infected blood or bodily fluids, which can occur through sex, injecting drugs, or during pregnancy or delivery.
The CDC’s previous recommendation was made in 2008 and urged testing for people at high risk. Now, the agency recommends screening for everyone 18 and older at least once. The agency continues to recommend that pregnant people be screened during each pregnancy, regardless of whether they’ve been vaccinated or tested in the past. People at high risk – including those who are incarcerated, have multiple sex partners or have a history of hepatitis C infection – should be tested periodically.
The symptoms of acute hepatitis B infection can include fever, fatigue, abdominal pain, dark urine and jaundice, among others; these signs can take months to appear and can last for weeks or months, but most people clear the infection. People who progress to develop chronic hepatitis B often feel fine and don’t have symptoms, sometimes for decades. But if symptoms do appear, they can look like the acute infection – and may be a sign of advanced liver disease.
Several medications are available to treat people with chronic hepatitis B. There is also a highly effective vaccine against hepatitis B.
“Although a curative treatment is not yet available, early diagnosis and treatment of chronic HBV infections reduces the risk for cirrhosis, liver cancer, and death,” the CDC said. “Along with vaccination strategies, universal screening of adults and appropriate testing of persons at increased risk for HBV infection will improve health outcomes, reduce the prevalence of HBV infection in the United States, and advance viral hepatitis elimination goals.”

|
From October 2021 through May 2022, approximately 109 cases of acute hepatitis of unknown origin in children were publicly reported.1 Since May 3, 2023, an additional 282 cases (391 total pediatric patients) have been reported in 46 states and jurisdictions and in at least 11 countries in Europe and the Americas.1 The recent increase in cases under investigation were identified retrospectively since October 1, 2021, and may not ultimately be linked to this investigation. No additional deaths have been reported since February 2023, and the proportion of patients requiring liver transplants has decreased from 15% to 9% from May 5, 2022, through May 3, 2023. Additional testing details were updated by the CDC on May 11, 2022. The CDC continues to investigate the cause and any contributing factors (e.g., immune response to adenovirus, coinfections, environmental exposures, medications) related to these pediatric hepatitis cases.1 Source |
spacer
Hepatitis C (HCV)
Hepatitis C is a contagious liver disease that ranges in severity from a mild illness lasting a few weeks to a serious lifelong illness that attacks the liver. infection is the result of the Hepatitis C virus (HCV) which is spread primarily through contact with the blood of an infected person. Hepatitis C can be either “acute” or “chronic.”
In 2018 there were an estimated 50,300 cases of acute Hepatitis C cases in the United States. An estimated 2.4 million people in the United States had chronic Hepatitis C between 2013 and 2016. More than 50% of people who beome infected with Hepatitis C will develop chronic infection. Today, most people become infected with the Hepatitis C virus by sharing needles or other equipment used to inject drugs.
The Hepatitis C virus can survive outside of the body at room temperature, on environmental surfaces, for up to 3 weeks.
Symptoms
Symptoms of acute Hepatitis C can include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain and more. However, 70%-80% of individuals infected with Hepatitis C have no symptoms. In many cases, there are no symptoms of the disease until liver problems have developed. Hepatitis C is often detected during routine blood tests to measure liver function and liver enzyme (protein produced by the liver) level. For more information review the CDC Fact Sheet.
Prevention
There is currently no vaccine for the prevention of HCV, research into the development of a vaccine is underway. For more information visit:CDC

Pseudomonas is a type of bacteria (germ) that is found commonly in the environment, like in soil and in water. Of the many different types of Pseudomonas, the one that most often causes infections in humans is called Pseudomonas aeruginosa, which can cause infections in the blood, lungs (pneumonia), or other parts of the body after surgery.
See CDC’s report
Antibiotic Resistance Threats in the United States, 2019
These bacteria are constantly finding new ways to avoid the effects of the antibiotics used to treat the infections they cause. Antibiotic resistance occurs when the germs no longer respond to the antibiotics designed to kill them. If they develop resistance to several types of antibiotics, these germs can become multidrug-resistant.
How common are these infections?
In 2017, multidrug-resistant Pseudomonas aeruginosa caused an estimated 32,600 infections among hospitalized patients and 2,700 estimated deaths in the United States [Source: 2019 AR Threats Report].
Who is at risk?
Those most at risk include patients in hospitals, especially those: on breathing machines (ventilators); with devices such as catheters; with wounds from surgery or burns.
How is it spread?
Pseudomonas aeruginosa lives in the environment and can be spread to people in healthcare settings when they are exposed to water or soil that is contaminated with these germs. Resistant strains of the germ can also spread in healthcare settings from one person to another through contaminated hands, equipment, or surfaces.
you avoid getting an infection?
Patients and caregivers should:
- keep their hands clean to avoid getting sick and spreading germs that can cause infections
- wash their hands with soap and water or use alcohol-based hand sanitizer, particularly before and after caring for wounds or touching a medical device
- remind healthcare providers and caregivers to clean their hands before touching the patient or handling medical devices
- allow healthcare staff to clean their room daily when in a healthcare setting
Healthcare providers should pay careful attention to recommended infection control practices, including hand hygiene and environmental cleaning (e.g., cleaning of patient rooms and shared equipment) to reduce the risk of spreading these germs to patients.
Healthcare facilities should have water management plans (see Reduce Risk from Water) that help ensure water quality and reduce the risk of exposure to potentially harmful germs like Pseudomonas aeruginosa.
How are these infections treated?
Pseudomonas aeruginosa infections are generally treated with antibiotics. Unfortunately, in people exposed to healthcare settings like hospitals or nursing homes, Pseudomonas aeruginosa infections are becoming more difficult to treat because of increasing antibiotic resistance.
To identify the best antibiotic to treat a specific infection, healthcare providers will send a specimen (often called a culture) to the laboratory and test any bacteria that grow against a set of antibiotics to determine which are active against the germ. The provider will then select an antibiotic based on the activity of the antibiotic and other factors, like potential side effects or interactions with other drugs. For some multidrug-resistant types of Pseudomonas aeruginosa, treatment options might be limited.
spacer
Key facts
- Mpox (monkeypox) is a viral illness caused by the monkeypox virus, a species of the genus Orthopoxvirus. Two different clades exist: clade I and clade II
- Common symptoms of mpox are a skin rash or mucosal lesions which can last 2–4 weeks accompanied by fever, headache, muscle aches, back pain, low energy, and swollen lymph nodes.
- Mpox can be transmitted to humans through physical contact with someone who is infectious, with contaminated materials, or with infected animals.
- Laboratory confirmation of mpox is done by testing skin lesion material by PCR.
- Mpox is treated with supportive care. Vaccines and therapeutics developed for smallpox and approved for use in some countries can be used for mpox in some circumstances.
- In 2022–2023 a global outbreak of mpox was caused by a strain known as clade IIb.
- Mpox can be prevented by avoiding physical contact with someone who has mpox. Vaccination can help prevent infection for people at risk.
Overview
Mpox (monkeypox) is an infectious disease caused by the monkeypox virus. It can cause a painful rash, enlarged lymph nodes and fever. Most people fully recover, but some get very sick.
Anyone can get mpox. It spreads from contact with infected:
|
|
If you have mpox:
|
|
The disease mpox (formerly monkeypox) is caused by the monkeypox virus (commonly abbreviated as MPXV), an enveloped double-stranded DNA virus of the Orthopoxvirus genus in the Poxviridae family, which includes variola, cowpox, vaccinia and other viruses. The two genetic clades of the virus are clades I and II.
The monkeypox virus was discovered in Denmark (1958) in monkeys kept for research and the first reported human case of mpox was a nine-month-old boy in the Democratic Republic of the Congo (DRC, 1970). Mpox can spread from person to person or occasionally from animals to people. Following eradication of smallpox in 1980 and the end of smallpox vaccination worldwide, mpox steadily emerged in central, east and west Africa. A global outbreak occurred in 2022–2023. The natural reservoir of the virus is unknown – various small mammals such as squirrels and monkeys are susceptible.
| Ok, let’s take a moment and look at this information. It is very revealing. First off, DENMARK part of the Netherlands where the UN was created and where it is still headquatered in the Tower of Bable next to the Harlot riding the Beast. Also, where the BEAST COMPUTER was created. The Monkeypos came out of the CONGO that just happened to be under rule of the Netherlands. And the first case was a helpless infant. A pagan sacrifice.
Note that once smallpox was no longer a threat and they had no longer had a way to impose the vaccine that had to come up with another threat and another poison injection. So Monkeypox was created to fill the bill. ALSO NOTE: That as soon as the COVID PLANDEMIC fizzled, they had to come up with a plan to control the masses while they worked on creating more variants….once again, MONKEYPOX to the rescue. Sounds like a crazy “CONSPIRACY THEORY” because it is a CRAZY CONSPIRACY!! NOT A THEORY! |
Transmission
Person-to-person transmission of mpox can occur through direct contact with infectious skin or other lesions such as in the mouth or on genitals; this includes contact which is
|
|
The virus then enters the body through broken skin, mucosal surfaces (e g oral, pharyngeal, ocular, genital, anorectal), or via the respiratory tract. Mpox can spread to other members of the household and to sex partners. People with multiple sexual partners are at higher risk.
Animal to human transmission of mpox occurs from infected animals to humans from bites or scratches, or during activities such as hunting, skinning, trapping, cooking, playing with carcasses, or eating animals. The extent of viral circulation in animal populations is not entirely known and further studies are underway.
People can contract mpox from contaminated objects such as clothing or linens, through sharps injuries in health care, or in community setting such as tattoo parlours.
Signs and symptoms
Mpox causes signs and symptoms which usually begin within a week but can start 1–21 days after exposure. Symptoms typically last 2–4 weeks but may last longer in someone with a weakened immune system.
Common symptoms of mpox are:
|
|
|
For some people, the first symptom of mpox is a rash, while others may have different symptoms first.
The rash begins as a flat sore which develops into a blister filled with liquid and may be itchy or painful. As the rash heals, the lesions dry up, crust over and fall off.
Some people may have one or a few skin lesions and others have hundreds or more. These can appear anywhere on the body such as the:
|
|
Some people also have painful swelling of their rectum or pain and difficulty when peeing.
People with mpox are infectious and can pass the disease on to others until all sores have healed and a new layer of skin has formed.
Children, pregnant people and people with weak immune systems are at risk for complications from mpox.
Typically for mpox, fever, muscle aches and sore throat appear first. The mpox rash begins on the face and spreads over the body, extending to the palms of the hands and soles of the feet and evolves over 2-4 weeks in stages – macules, papules, vesicles, pustules. Lesions dip in the centre before crusting over. Scabs then fall off. Lymphadenopathy (swollen lymph nodes) is a classic feature of mpox. Some people can be infected without developing any symptoms.
In the context of the global outbreak of mpox which began in 2022 (caused mostly by Clade IIb virus), the illness begins differently in some people. In just over a half of cases, a rash may appear before or at the same time as other symptoms and does not always progress over the body. The first lesion can be in the groin, anus, or in or around the mouth.
People with mpox can become very sick. For example, the skin can become infected with bacteria leading to abscesses or serious skin damage. Other complications include pneumonia, corneal infection with loss of vision; pain or difficulty swallowing, vomiting and diarrhoea causing severe dehydration or malnutrition; sepsis (infection of the blood with a widespread inflammatory response in the body), inflammation of the brain (encephalitis), heart (myocarditis), rectum (proctitis), genital organs (balanitis) or urinary passages (urethritis), or death. Persons with immune suppression due to medication or medical conditions are at higher risk of serious illness and death due to mpox. People living with HIV that is not well-controlled or treated more often develop severe disease.
Diagnosis
Identifying mpox can be difficult as other infections and conditions can look similar. It is important to distinguish mpox from chickenpox, measles, bacterial skin infections, scabies, herpes, syphilis, other sexually transmissible infections, and medication-associated allergies. Someone with mpox may also have another sexually transmissible infection such as herpes. Alternatively, a child with suspected mpox may also have chickenpox. For these reasons, testing is key for people to get treatment as early as possible and prevent further spread.
Detection of viral DNA by polymerase chain reaction (PCR) is the preferred laboratory test for mpox. The best diagnostic specimens are taken directly from the rash – skin, fluid or crusts – collected by vigorous swabbing. In the absence of skin lesions, testing can be done on oropharyngeal, anal or rectal swabs. Testing blood is not recommended. Antibody detection methods may not be useful as they do not distinguish between different orthopoxviruses.
More information on laboratory confirmation of mpox can be found here.
Treatment and vaccination
The goal of treating mpox is to take care of the rash, manage pain and prevent complications. Early and supportive care is important to help manage symptoms and avoid further problems.
Getting an mpox vaccine can help prevent infection. The vaccine should be given within 4 days of contact with someone who has mpox (or within up to 14 days if there are no symptoms).
It is recommended for people at high risk to get vaccinated to prevent infection with mpox, especially during an outbreak. This includes:
|
|
Persons who have mpox should be cared for away from other people.
Several antivirals, such as tecovirimat, originally developed to treat smallpox have been used to treat mpox and further studies are underway. Further information is available on mpox vaccination and case management.
Self-care and prevention
Most people with mpox will recover within 2–4 weeks. Things to do to help the symptoms and prevent infecting others:
Do
|
|
|
Do not
|
|
To prevent spread of mpox to others, persons with mpox should isolate at home, or in hospital if needed, for the duration of the infectious period (from onset of symptoms until lesions have healed and scabs fall off). Covering lesions and wearing a medical mask when in the presence of others may help prevent spread. Using condoms during sex will help reduce the risk getting mpox but will not prevent spread from skin-to-skin or mouth-to-skin contact.
Outbreaks
After 1970, mpox occurred sporadically in Central and East Africa (clade I) and West Africa (clade II). In 2003 an outbreak in the United States of America was linked to imported wild animals- Monkeys used for lab experiments (clade II). Since 2005, thousands of suspected cases are reported in the DRC every year. In 2017, mpox re-emerged in Nigeria and continues to spread between people across the country and in travellers to other destinations. Data on cases reported up to 2021 are available here.

In May 2022, an outbreak of mpox appeared suddenly and rapidly spread across Europe, the Americas and then all six WHO regions, with 110 countries reporting about 87 thousand cases and 112 deaths. The global outbreak has affected primarily (but not only) gay, bisexual, and other men who have sex with men and has spread person-to-person through sexual networks. More information on the global outbreak is available here with detailed outbreak data here;
In 2022, outbreaks of mpox due to Clade I MPXV occurred in refugee camps in the Republic of the Sudan. A zoonotic origin has not been found. Very interesting, in refugee camps the ruling elite control everything. The zoonotic origin was in a LAB! NO ONE IS GOING TO TALK ABOUT THAT!
WHO response
The global outbreak of mpox was declared a public health emergency of international concern (PHEIC) on 23 of July 2022. WHO published a strategic preparedness and response plan for mpox and a suite of technical guidance documents. Surveillance, diagnostics, risk communication and community engagement remain central to stopping the outbreak and eliminating human-to-human transmission of mpox in all contexts.
More information can be found here. Questions and answers are here and public health advice is here.
spacer
The World Health Organization on May 11 said mpox no longer presents a public health emergency of international concern because global cases have declined and countries are better equipped to respond, but that doesn’t mean the threat is eliminated. Last year’s mpox outbreak started in the spring, driven in part by festivals, pride events and other celebrations popular among gay men where attendees are traveling and having sex with new partners.
The Centers for Disease Control and Prevention on May 19 warned of a “substantial” risk of renewed mpox outbreaks in the United States and has issued alerts warning health providers to be vigilant.
Public health authorities aren’t expecting a repeat of last year’s explosion of cases, more than 30,000 in the United States and 87,000 globally, because of greater awareness and widespread vaccination and protection from earlier infections. But smaller scale outbreaks are still possible, including in those with some immunity. Officials warned last year that they could not say how long protection against mpox from the Jynneos vaccine would last.
How many mpox cases are there?
There’s no sign of a U.S. resurgence of mpox, which is now a sporadic event. The seven-day average of new cases has remained below four since early February, according to the CDC.
But the Chicago Department of Public Health has issued an alert warning of a local resurgence. The agency has reported 21 cases in recent weeks, including 12 people who were fully vaccinated and five who were partially vaccinated. Most were men who have sex with men, consistent with past outbreaks. The breakthrough cases appear mild, which experts say is a sign that vaccines are preventing serious illness.
“CDPH continues to stress that while vaccination will not make someone 100 percent immune to mpox, it’s still an important tool to stop the spread of the virus,” the agency said in a statement. “People who are vaccinated still should continue to avoid close, skin-to-skin contact with someone who has mpox.”
Experts say the Chicago cases should prompt others to remain vigilant.
“We know that mpox has fallen off the radar due to months without any cases being reported in multiple jurisdictions across the U.S., but with this cluster popping up, it needs to be brought to the forefront again,” said Joseph Cherabie, associate medical director of the St. Louis County Sexual Health Clinic in Missouri.
Does the mpox vaccine work?
Three studies released May 18 showed a wide range of estimates for the effectiveness of the Jynneos vaccine, the only licensed mpox vaccine in the United States. They show robust but imperfect protection from two doses and lower effectiveness from one dose. But they do not show long how protection lasts — a question other ongoing studies aim to answer.
|
Fenit Nirappil
@FenitN
A wide range in the Jynneos vaccine effectiveness estimates released yesterday. CDC officials said this kind of variation isn’t surprising but the overall takeaway is vaccines offer protection against mpox and two shots are better than one
|
About 1.6 million people are considered at-risk for mpox, but only 37 percent have received at least one shot, and 23 percent have received both shots. Public health officials say news of vaccinated people getting mpox shouldn’t dissuade people from getting shots. They draw comparisons to coronavirus vaccines — which are not foolproof against infections, but reduce severity of disease.
Now is the time to get vaccinated for optimal protection ahead of Pride and summer because shots are supposed to be administered at least four weeks apart, and full protection comes 14 days after the second shot.
“Our best defense is a good offense, and the more people we get vaccinated, even with a vaccine that doesn’t have 100 percent protection, the more likely we are to control mpox,” Daskalakis said.
Third shots as booster doses or vaccines in people who have been previously infected are not recommended.
Dengue cases in the US
- Dengue virus disease became a nationally notifiable condition in 2010.
- Cases are reported to CDC by state, territorial, and local health departments using standard case definitions.
Provisional data* as of August 2, 2023
This webpage contains provisional data reported to ArboNET for 2023.
US States
- 225 dengue cases reported
US Territories
- 315 dengue cases reported
States and territories reporting dengue cases – United States, 2023 (as of August 2, 2023)
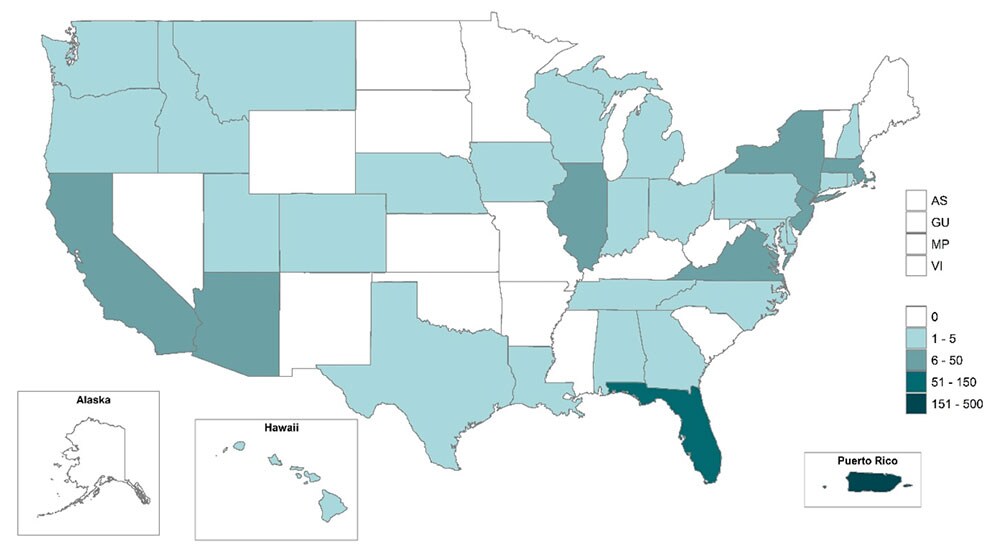 *CDC reports provisional dengue case counts reported to ArboNET for the United States and its territories on the first Thursday of each month.
*CDC reports provisional dengue case counts reported to ArboNET for the United States and its territories on the first Thursday of each month.
Table 1: Dengue cases reported to ArboNET by state or territory of residence – United States, 2023 (as of August 2, 2023)
| Travel-associated cases No. (%) |
Locally-transmitted cases No. (%) |
|
|---|---|---|
| State | (N=222) | (N=3) |
| Alabama | 2 (1) | 0 (0) |
| Arizona | 9 (4) | 0 (0) |
| California | 11 (5) | 0 (0) |
| Colorado | 4 (2) | 0 (0) |
| Connecticut | 1 (0) | 0 (0) |
| Delaware | 1 (0) | 0 (0) |
| Florida | 96 (43) | 2 (67) |
| Georgia | 1 (0) | 0 (0) |
| Hawaii | 2 (1) | 0 (0) |
| Idaho | 1 (0) | 0 (0) |
| Illinois | 10 (5) | 0 (0) |
| Indiana | 1 (0) | 0 (0) |
| Iowa | 2 (1) | 0 (0) |
| Louisiana | 1 (0) | 0 (0) |
| Maryland | 2 (1) | 0 (0) |
| Massachusetts | 12 (5) | 0 (0) |
| Michigan | 1 (0) | 0 (0) |
| Montana | 1 (0) | 0 (0) |
| Nebraska | 2 (1) | 0 (0) |
| New Hampshire | 1 (0) | 0 (0) |
| New Jersey | 13 (6) | 0 (0) |
| New York | 23 (10) | 0 (0) |
| North Carolina | 2 (1) | 0 (0) |
| Ohio | 3 (1) | 0 (0) |
| Oregon | 1 (0) | 0 (0) |
| Pennsylvania | 5 (2) | 0 (0) |
| Rhode Island | 2 (1) | 0 (0) |
| Tennessee | 2 (1) | 0 (0) |
| Texas | 0 (0) | 1 (33) |
| Utah | 1 (0) | 0 (0) |
| Virginia | 7 (3) | 0 (0) |
| Washington | 1 (0) | 0 (0) |
| Wisconsin | 1 (0) | 0 (0) |
| Travel-associated cases No. (%) |
Locally-transmitted cases No. (%) |
|
|---|---|---|
| Territories | (N=1) | (N=314) |
| Puerto Rico | 1 (100) | 314 (100) |
DENGUE OUTBREAKS 2023
Dengue Outbreaks August 2023
According to the U.S. Centers for Disease Control and Prevention (CDC), dengue is a vaccine-preventable, vectorborne infectious disease caused by four dengue viruses and is endemic in about 125 countries. Dengue is present in Asia, the Pacific Islands, the Caribbean, the Americas, Africa, and Mexico. The CDC recently issued Travel Health Notices regarding dengue outbreaks in the Americas (2023), Africa/Middle East (July 21, 2023), Costa Rica, and Asia/Pacific Islands (July 25, 2023). In addition, the Pan American Health Organization (PAHO) and the World Health Organization (WHO) issued various dengue travel advisories in 2023. And the European Centre for Disease Prevention and Control (ECDC) says about 400 million dengue infections occur yearly.
The Annals of Internal Medicine published results from a study on June 20, 2023, which found most dengue patients acquired the disease in the Caribbean (31%) and Southeast Asia (24%). And a recent study published by the Royal Society indicates that dengue-carrying mosquitoes are expanding their range by an average of 6.5 meters of elevation and have moved polewards by 4.7 km annually. Dengue infections are detectable by approved tests offered by Ulta Labs.
Dengue Mexico
Dengue has been reported in 28 of 32 Mexico states in 2023. Quintana Roo is the leading state reporting Dengue cases in 2023. In 2022, the PAHO reported 36,926 cases throughout Mexico and 53 dengue deaths (Sonora confirmed 14 deaths, Oaxaca 13 deaths). In addition, dengue transmission has been documented in Yucatan, Mexico (Cancun) since 1979. The recent increase in dengue cases in Mexico has been partly attributed to the genetic diversification of DENV serotypes and the emergence of new genotypes across Latin America (Hernández-García et al., 2020).
Dengue United States

Provisional data published by the U.S. CDC as of August 2, 2023, indicates U.S. states (Florida, New York, Illinois, and Arizona) reported about 222 travel-related (most from Cuba) and (3) locally-acquired dengue cases in Florida (2) and Texas (1). In addition, the CDC says dengue is endemic in the U.S. territories of Puerto Rico, American Samoa, the U.S. Virgin Islands (USVI), the Federated States of Micronesia, the Republic of Marshall Islands, and the Republic of Palau.
As of July 29, 2023, the Florida Health Department reported as of week #30, there had been 147 travel-associated dengue cases and six locally acquired dengue cases confirmed in 2023. In 2022, 903 travel-associated and 68 locally-acquired dengue cases were reported. Miami-Dade County remains under a mosquito-borne illness alert. In 2022, the Florida Department of Health in Miami-Dade County confirmed (DENV-3) cases, and in Broward County, a mosquito-borne illness alert was issued.
As of July 27, 2023, Puerto Rico’s Department of Health Arboviral Disease Week #28 report indicates about 383 probable dengue cases in 2023. In 2022, 929 confirmed dengue cases and three related fatalities were reported. From 2010 to 2020, approximately 95% of locally acquired dengue cases in the U.S. (n = 31,289) occurred near San Juan, Puerto Rico (n = 29,779). The estimated dengue seroprevalence among persons nine years of age was approximately 40%. During 2010–2020, Puerto Rico reported the highest number of dengue cases (29,862 [96.6%]), followed by American Samoa (660), USVI (353), and Guam (28). A recent CDC study stated that dengue vaccinations’ cost-effectiveness in PR depends on the seroprevalence, which is lower for younger age groups.
Recent investigations reported on CDC.gov
- Ground Beef – Salmonella InfectionsANNOUNCED JULY 2023
- Suspected Fungal Meningitis – Epidural Related Surgeries in MexicoANNOUNCED MAY 2023
- Backyard Poultry – Salmonella InfectionsANNOUNCED MAY 2023
- Drug-resistant Infections Associated with Artificial TearsANNOUNCED FEBRUARY 2023
Ok, My Comments so far.
I have wanted to say these things from the top of the post, but I decided it was best for you to see the data for yourself first.
Several things that you probably already noticed in the information above:
- They are clearly focused on collecting data to feed into their AI learning system. Anything you say to medical personnel, any responses you give to them, anything you write down on a questionnaire, any question you ask while you are in their office or speaking to them on the phone is put into the database and becomes a part of your permanent record. Along with any observations or judgements the medical staff make. NOTHING IS PRIVATE ANYMORE. The only ones who have trouble getting information from your record is YOU or anyone you need to get it to.
2. They are pushing medical treatment and vaccinations for diseases you may not ever get and ones that are most often easily treated at home. Handled by your natural immune system, along with bed rest, lots of liquids, a good diet and exercise.
3. I am sure you were as shocked as I was to see how VERY LOW the Numbers of Cases were for nearly every disease we reviewed above! NONE of those should have been considered an outbreak let alone endemic or pandemic. Nor do they require surveillance of the public.
Those are things I am sure you noticed. I have a few more things to say before we move on.
They want you to seek medical treatment for everything. But, once you get the medical industry involved, it is like once you get the police involved in your private affairs. You place yourself under their authority. Opening yourself up for further surveillance, further treatments, further “recommendations” and perhaps even separation from your family and your home, at their discretion. In this crazy world, that is not a great plan.
Once you arrive at a medical facility, you have lost control They can decide to keep you. They can decide that you need treatments you may or may not like, or want to submit to.
As you have seen, most of these diseases do not require medical intervention. Certainly, you don’t need to expose yourself to the risks involved with vaccinations for a disease you may not, probably won’t ever even get!’
The side effects and unknown dangers of their vaccines are far worse than any disease. AND, what they call vaccines today are not vaccines. They are DNA therapy that destroys your natural immune system!
The vaccines are their weapon to gain control of everyone. They already have a schedule of vaccines planned and mandated for every age group. They are not yet enforcing it… but they will. They have already been given the authority to mandate whatever they decide is “necessary”. Once they make all the vaccines mandatory, they will FORCE COMPLIANCE. Anyone who does not comply will be dealt with severely. You may lose your job, or your SSI payments, or your healthcare, or your right to buy food, you may lose your residence and be out on the street. Or they may incarcerate you, or just kill you outright. NO JOKE FOLKS!
spacer
Coronavirus Update

World Health Organization Director-General Tedros Adhanom Ghebreyesus has upgraded EG.5 to a variant of interest and urged countries to continue their surveillance of COVID.
A
eg – Wiktionary, the free dictionary
| edge (n.) |
|
a : the line where an object or area begins or ends : BORDER on the edge of a plain b : the narrow part adjacent to a border the edge of the deck d : a favorable margin : ADVANTAGE has an edge on the competition
|
|
harrow · noun. an agricultural implement with spikelike teeth or upright disks, drawn chiefly over plowed land to level it, break up clods, root up weeds, etc.
|
|
(military) An obstacle formed by turning an ordinary harrow upside down, the frame being buried so that it is unseen.
|
Harrow – Definition, Meaning & SynonymsVocabulary.com
To harrow is to cause worry and upset, the way a truly scary movie might harrow you, making it hard to sleep without turning on the light.
|
| harrow |
harrow – wiktionary Verbharrow (third-person singular simple present harrows, present participle harrowing, simple past and past participle harrowed)
|
Eris (/ˈɪərɪs,ˈɛrɪs/; Greek: Ἔρις Éris, “Strife”) is the Greek goddess of strife and discord. Her Roman equivalent is Discordia, which means the same. Eris’s Greek opposite is Harmonia, whose Roman counterpart is Concordia,[3] though she is also described as opposing Nike, counterpart of the Roman Victoria. Homer equated her with the war-goddess Enyo, whose Roman counterpart is Bellona. The dwarf planet Eris is named after the goddess.
She had no temples in ancient Greece and functions essentially as a personification, as which she appears in Homer and many later works.
Etymology
Eris is of uncertain etymology; connections with the verb ὀρίνειν orínein, ‘to raise, stir, excite’, and the proper name Ἐρινύες Erinyes have been suggested. R. S. P. Beekes rejects these derivations and suggested a Pre-Greek origin.[4]
Characteristics in Greek mythology
In Hesiod‘s Works and Days 11–24, two different goddesses named Eris are distinguished:
So, after all, there was not one kind of Strife alone, but all over the earth there are two. As for the one, a man would praise her when he came to understand her; but the other is blameworthy: and they are wholly different in nature. For one fosters evil war and battle, being cruel: her no man loves; but perforce, through the will of the deathless gods, men pay harsh Strife her honour due.
(Nyx), and the son of Cronus [i.e. Zeus] who sits above and dwells in the aether, set her in the roots of the earth: and she is far kinder to men. She stirs up even the shiftless to toil; for a man grows eager to work when he considers his neighbour, a rich man who hastens to plough and plant and put his house in good order; and neighbour vies with his neighbour as he hurries after wealth. This Strife is wholesome for men.And potter is angry with potter, and craftsman with craftsman and beggar is jealous of beggar, and minstrel of minstrel.
(Hesiod, Works and Days, 120-130)
Strife is no only child. Upon the earth
Two strifes exist; the one is praised by those
Who come to know her, and the other blamed.
Their natures differ: for the cruel one
Makes battles thrive, and war; she wins no love
But men are forced, by the immortals‘ will,
To pay the grievous goddess due respect.
The other, first-born child of blackest Night,
Was set by Zeus, who lives in air, on high,
Set in the roots of earth, an aid to men.
She urges even lazy men to work.
In Hesiod’s Theogony (226–232), Eris, the daughter of Night, is less kindly spoken of as she brings forth other personifications as her children:
And hateful Eris bore painful Ponos (Hardship),
Lethe (Forgetfulness) and Limos (Starvation) and the tearful Algea (Pains),
Hysminai (Battles), Makhai (Wars), Phonoi (Murders), and Androktasiai (Manslaughters);
Neikea (Quarrels), Pseudea (Lies), Logoi (Stories), Amphillogiai (Disputes),
Dysnomia (Anarchy) and Ate (Ruin), near one another,
and Horkos (Oath), who most afflicts men on earth,
Then willing swears a false oath.[5]
The other Eris is presumably she who appears in Homer‘s Iliad Book IV; equated with Enyo as sister of Ares and so presumably daughter of Zeus and Hera:[6]
… and Discord [Ἔρις] that rageth incessantly, sister and comrade of man-slaying Ares; she at the first rears her crest but little, yet thereafter planteth her head in heaven, while her feet tread on earth. She it was that now cast evil strife into their midst as she fared through the throng, making the groanings of men to wax.[7]
She also has a son whom she named Strife.
Enyo is mentioned in Book 5, and Zeus sends Strife to rouse the Achaeans in Book 11, of the same work.
The most famous tale of Eris recounts her initiating the Trojan War by causing the Judgement of Paris. The goddesses Hera, Athena and Aphrodite had been invited along with the rest of Olympus to the forced wedding of Peleus and Thetis, who would become the parents of Achilles, but Eris had been snubbed because of her troublemaking inclinations.
She therefore (as mentioned at the Kypria according to Proclus as part of a plan hatched by Zeus and Themis) tossed into the party the Apple of Discord, a golden apple inscribed Ancient Greek: τῇ καλλίστῃ, romanized: tē(i) kallistē(i) – “For the most beautiful one”, or “To the Fairest One” – provoking the goddesses to begin quarreling about the appropriate recipient. The hapless Paris, Prince of Troy, was appointed to select the fairest by Zeus. The goddesses stripped naked to try to win Paris’s decision, and also attempted to bribe him. Hera offered political power; Athena promised infinite wisdom; and Aphrodite tempted him with the most beautiful woman in the world: Helen, wife of Menelaus of Sparta. While Greek culture placed a greater emphasis on prowess and power, Paris chose to award the apple to Aphrodite, thereby dooming his city, which was destroyed in the war that ensued.
Eris is also mentioned in Nonnus‘s Dionysiaca, when Typhon prepares to battle with Zeus:
Eris (“Strife”) was Typhon’s escort in the mellay, Nike (“Victory”) led Zeus into battle.[8]
Another story of Eris includes Hera, and the love of Polytechnus and Aedon. Polytechnos and Aëdon lived a prosperous life with their son, Itys.
| -itis |
They claimed to love each other more than Hera and Zeus were in love. This angered Hera, so she sent Eris to wreak discord upon them. Polytekhnos was finishing off a chariot board, and Aedon a web she had been weaving. Eris said to them, “Whosoever finishes thine task last shall have to present the other with a female servant!” Aedon won. But Polytekhnos was not happy by his defeat, so he came to Khelidon, Aedon’s sister, and raped her. He then disguised her as a slave, presenting her to Aedon. When Aedon discovered this was indeed her sister, she chopped up Polytekhnos’s son and fed him to Polytekhnos. The gods were not pleased, so they were transformed into birds.[9]
|
from Greek polytekhnos “skilled in many arts,” from polys “many” (from PIE root *pele- (1) “to fill”) + tekhnē “art” (see techno-). As a noun (short for polytechnic institution) from 1836. Related: Polytechnical. |
|
techno-
word-forming element meaning “art, craft, skill,” later “technical, technology,” from Latinized form of Greek tekhno-, combining form of tekhnē “art, skill, craft in work; method, system, an art, a system or method of making or doing,” from PIE *teks-na- “craft” (of weaving or fabricating), from suffixed form of root *teks- “to weave,” also “to fabricate.” fabricate – Wiktionary, the free dictionary *teks-
Proto-Indo-European root meaning “to weave,” also “to fabricate,” especially with an ax, also “to make wicker or wattle fabric for (mud-covered) house walls.” |
Eris has been adopted as the patron deity of the modern Discordian religion, which was begun in the late 1950s by Gregory Hill and Kerry Wendell Thornley under the pen names of “Malaclypse the Younger” and “Omar Khayyam Ravenhurst”. The Discordian version of Eris is considerably lighter in comparison to the rather malevolent Graeco-Roman original, wherein she is depicted as a positive (albeit mischievous) force of chaotic creation. Principia Discordia, the first holy book of Discordianism, states:
The story of Eris being snubbed and indirectly starting the Trojan War is recorded in the Principia, and is referred to as the Original Snub. The Principia Discordia states that her parents may be as described in Greek legend, or that she may be the daughter of Void. She is the Goddess of Disorder and Being, whereas her sister Aneris (called the equivalent of Harmonia by the Mythics of Harmonia) is the goddess of Order and Non-Being. Their brother is Spirituality.[11]
Discordian Eris is looked upon as a foil to the preoccupation of western philosophy in attempting find order in the chaos of reality, in prescribing order to be synonymous with truth. Discordian Eris teaches us that the only truth is chaos, and that order and disorder are simply temporary filters applied to the lenses we view the chaos through. This is known as the Aneristic Illusion.[12]
In this telling, Eris becomes something of a patron saint of chaotic creation:
I am chaos. I am the substance from which your artists and scientists build rhythms. I am the spirit with which your children and clowns laugh in happy anarchy. I am chaos. I am alive, and I tell you that you are free.[13]
The concept of Eris as developed by the Principia Discordia is used and expanded upon in the science fiction work The Illuminatus! Trilogy by Robert Shea and Robert Anton Wilson (in which characters from Principia Discordia appear). In this work, Eris is a major character.[14]
The classic fairy tale “Sleeping Beauty“ is partly inspired by Eris’s role in the wedding of Peleus and Thetis. Like Eris, a malevolent fairy curses a princess after not being invited to the princess’s christening.[15][16]
spacer
CULTURE JAMMING & DISCORDIANISM EXPLAINED – AUTUMN TYR-SALVIA
THE PRANKSTER HAS BECOME the PROPHET!
spacer

Nature & Appearance
Throughout Greek mythology, Eris is portrayed as a mean figure and a troublemaker. She is avoided by many of her fellow gods and goddesses.The only god who can tolerate her is her brother Ares, who often rides into battle with her and rejoices in the horrors of war alongside her. In the Iliad, Homer mentions that she often strides across the earth, spreading hate against both the Trojan and Greek armies. Unlike Ares, who eventually sided with the Trojans, Eris never took a side during the Trojan War. In Book 11, Zeus sent Eris to Odysseus‘ ship, where she cried out in her terrible and great voice, raising the fighting spirit in each Greek soldier’s heart and effectively stopping them from sailing back home. At one point in the Iliad, Eris is the only one of the gods who stays on the battlefield to watch the battle, exalting in the bloodshed and entirely in her element.
Discordianism
Discordianism is a form of modern paganism that is goddess focused. The religion has grown over the years through word of mouth, role-playing clubs, the internet and the underground publishing industry. Its primary holy scripture is the Principia Discordia, written mainly by Gregory Hill. It describes how the religion began with a vision of Eris, who showed them a yin–yang-like symbol with the Apple of Discord on one side and a pentagon on the other. It tells the story of how humanity fell from grace due to the Original Snub (the wedding of Peleus and Thetis). The Apple of Discord established the Discordian Mysteries, including the Law of Fives, which teaches that all the events in the universe revolve around the number five. It involves the Five Commandments, the Five Apostles of Eris, and the Five-Fingered Hand of Eris, which guides all of humankind’s chaotic decisions and movements.
spacer
 The Five Fingered Hand of Eris
The Five Fingered Hand of Eris
Here we see the original illustration of the Five Fingered Hand of Eris from the Principia Discordia.
Quoth the Principia:
“The official symbol of POEE is here illustrated. It may be this, or any similar device to represent TWO OPPOSING ARROWS CONVERGING INTO A COMMON POINT. It may be vertical, horizontal, or else such, and it may be elaborated or simplified as desired.
“The esoteric name for this symbol is THE FIVE FINGERED HAND OF ERIS, commonly shortened to THE HAND.”
There is a movement afoot to adopt a stylized version of this glyph as the official symbol of the planet Eris, an effort the powers that be at Hexnet.org enthusiastically endorse fnord.
The hexagonal implications of this design are obvious and far-reaching. Clearly, the overall design is hexagonal, in that there are six protrusions from a central origin, along three axes of symmetry. Additionally though, the general structure as described in the Principia, consisting of two connecting arrows, is itself very hexagonal, in that the arrow is a form of trigonal archetype, and two triangles, added together, invariably form a hexagon. (Or some sort of lopsided quadrilateral. But ideally a hexagon.)
Why this is a five fingered hand and not a six fingered hand is a matter open to debate. Clearly, we have five fingers, but they are connected to an arm—so perhaps one of the six protrusions is an arm. Or perhaps the horizontal axis counts as one “finger” in both directions. It is indeed a mystery. However, it is interesting that, even with their penchant for fives, the the early Discordian fathers could not bring themselves to adopt a five-sided symbol for their cause. The pentagram remains a symbol for “aneristic” order, while the six-sided, hexagonal, and “organic” Hand remains the symbol of balance and vitality between the opposing forces of order and disorder. This is consistent with the use of hexagons elsewhere in modern symbolism, where they almost invariably represent principles of balance, harmony, symmetry, et cetera.
The “Five-Fingered Hand of Eris,” a holy symbol in Discordianism originally derived from the crescent shape of the Greek Epsilon
because 5is such an unpredictable number, it can representative of chaos and instability source
The number 5
The number 5 is used in the scriptures to point to the death of man. It is the number of death. Source
spacer
What is the vibration of 5?
The vibration of 5 is freedom-focused. The vibration to seek freedom mixes with number 5’s strong independence and restlessness. The number 5 seeks freedom from boundaries and beliefs set forth by society, government, religion, or educational settings. As the number 5 indicates a strong vibrational frequency around prioritizing freedom, it’s naturally bold, compelling, and often rebellious. The number 5 further expresses its vibration by looking for ways to express personal freedom—leading to a heightened vibration of curiosity and adventure.
Properties of the number 5
Symbolism
- It is the number of the harmony and the balance. It is also the number of the divine grace.
- The number 5 is a characteristic of the man. First, according to the Cabal, it is the number of the perfect Man (got rid from his animal side). According to the Bible, it is the symbol of the Man-God by the five wounds of the Christ on cross (for this reason, it is also considered as the number of the grace). But it is also associated to the man in general (2 + 3) having an unstable character of duality, 2, in spite of his divinity, 3. The 5 is also found on the human body: the five fingers of the hand and feet, the five senses (touch, taste, sense of smell, hearing and the sight), the five members (two arms, two legs and the head, the bust being the center), the five bones forming the metacarpus, the metatarse and the brain-pan, etc.
- Considerated as the mediator between God and the universe, the five is regarded as a symbol of the universe.
- Symbol of the will’s divine.
- Symbol of the perfection in the Mayas.
- Symbol of the incarnated conscience – 4, Matter, + 1, Spirit.
- Symbolize the force and the limits of the man in his control on the Universe.
- According to Thibaut Of Langres, the number 5 is attributed to the world for some reasons. First because the world is moved following a circular movement, just as the 5 when we multiply it by itself or by the other odd ones returns periodically. Also it is called in this sense “periodical”. Five years make a lustre, from “lustrare” which means “to make the turn”. On the other hand, 5 is attributed to the world due to the fact that it is composed of the first even and odd, 2 and 3. The world indeed, that is to say the whole of things, increases by the male and the female – even is female and odd male.
- In China, it is the number of the Center in addition to be considered as a male number amulet.
- Number of the life and the nature, according to Aeppli.
- Being the sum or rather the union of the first female number and the first male number, it is the symbol of creative life and erotic love according to Jung. But this one interprets also this number as that of the revolt.
- A nuptial number for the Etruscans and Romans because it is the first number resulting from the addition the first female number and the first male number. For the same reason, C. Agrippa calls it the number of the marriage.
- For H.- P. Blavatsky, “5 is the spirit of life and human love.”
Bible
- The five wounds of Jesus on the cross.
- The five parts of the clothing remaining of Jesus during his crucifixion after the soldiers had made four parts of his dress, plus his tunic which they did not tear. (Jn 19,23)
- Saint Paul declares that by five times he received the 39 lashes from the Jews. (2 Co 11,24)
- The five mad and wise virgins of the parable of Jesus. (Mt 25,1)
- The five porticos of the pool of Bethesda. (Jn 5,2)
- The five pebbles which made it possible to small king David to kill the giant Goliath.
- The five kinds of animals that God asked Abraham to present to him to conclude with him an alliance: a heifer of three years old, a goat of three years old, a ram of three years old, a turtledove and a young dove. (Gn 12, 5-18)
- The five books of the Torah (the Law) according to the Judaism that corresponds to the number of the first books of the Bible. The book of the Lamentations of Jeremiah contains also five chapters.
Gematria
- Numerical value of the Hebrew letter He (the Not-Me) representing the passive principle by excellence. This letter represents, according to Charrot, “a solar ray pouring on the earth its beneficial rain of life” and it symbolizes the universal life, the breath of the man, the air, the spirit, the soul, all what is stimulating and vivifying. For the cabalist Eleazar of Worm, the letter “He” symbolizes “the breath” .
SPACER
POEE (Pronounced “POEE”)
from Principia Discordia
POEE is a Non-prophet Irreligious Disoraganisation founded by Malaclypse the Younger and Omar Khayyam Ravenhurst.
POEE stands for Paratheo-Anametamystikhood Of Eris Esoteric. The first part can be taken to mean “equivalent deity, reversity beyond-mystique.” We are not really esoteric, it’s just that nobody pays much attention to us.
The POEE HEAD TEMPLE is the Joshua Norton Cabal of The Discordian Society, which is located in Mal-2’s pineal gland and can be found by temporally and spatially locating the rest of Mal-2.
POEE has no treasury, no by-laws, no articles, no guides save Mal-2’s pineal gland, and has only one scruple–which Mal-2 keeps on his key chain.
POEE has not registered, incorporated, or otherwise chartered with the State, and so the State does not recognize POEE or POEE Ordinations, which is only fair, because POEE does not recognize the State.POEE has 5 DEGREES:
There is the neophyte, or LEGIONNAIRE DISCIPLE. The LEGIONNAIRE DEACON, who is catching on. An Ordained POEE PRIEST/PRIESTESS or a CHAPLAIN. The HIGH PRIEST, the Polyfather. And POEE POPE.
POEE LEGIONNAIRE DISCIPLES are authorized to initiate others as Discordian Society Legionnaires. PRIESTS appoint their own DEACONS. The POLYFATHER ordains Priests. I don’t know about the POPES.—Malaclypse the Younger, Principia Discordia, Page 00022
According to the Principia Discordia, POEE is “a tribe of philosophers, theologians, magicians, scientists, artists, clowns, and similar maniacs who are intrigued by Eris goddess of confusion and her doings.” Furthermore it states that “POEE subscribes to the Law of Fives of Omar’s sect” and “POEE also recognizes the Holy 23.”
Paratheo-Anametamystikhood can be taken to mean “equivalent deity, reversing beyond-mystique”. Loosely interpreted, it basically states that “all deities are equivalent, there is no great mystery about that“.SPACER
OUTLINING OUR ENSLAVEMENT – DISCORDIANISM – CHURCH OF ERIS 420 EPISODE
SPACER
DISCORDIANISM & THE ONE WORLD ORDER (WEISHAUPT & BAUER’S 25 POINT PLAN)
SPACER
MORE INFORMATION ON THIS SUBJECT CAN BE FOUND IN THE FOLLOWING POSTS:
CRISPR – Part 1- GENETIC MANIPULATION the Springboard
CRISPR – Part 2- The DESTROYER
CRISPR – Part 3- THE ULTIMATE END
CRISPR – Part 4 – Unleashed
CRISPR-WUHAN VIRUS-WAKE UP and READ THE SIGNS!
Is there a Pandemic? IS Mandatory Vaccines the Answer?
Gifts from the Fallen – Part 6 – Vaccines
PANDEMIC – OUTBREAK – Diseases, Epidemics, Pandemics and Plagues
AT SIXES AND SEVENS!!
What do Vaccine Decliners Know that YOU DON’T??
VACCINE IS THE GAME-CHANGER – BEWARE
Official Swiss Study: Heart Defects From COVID Jabs Is 3,000 Times Higher Than Thought
Scientists Warn That Vaxx-Related ‘Turbo Cancers’ Are Contagious: “It’s Behaving Like a Bioweapon”



 Karen Weintraub
Karen Weintraub


/cloudfront-us-east-1.images.arcpublishing.com/gray/VU4M2UPA7BGN5CXIECIDGEFNPQ.jpg)